Page 143 - Read Online
P. 143
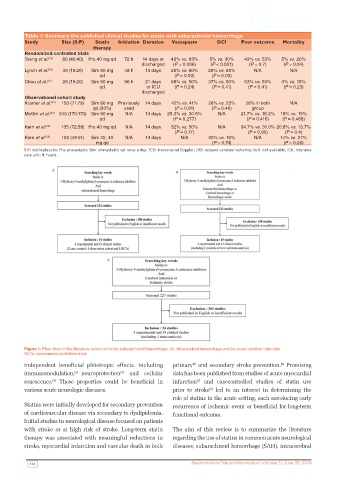
Table 1: Summary the published clinical studies for statin with subarachnoid hemorrhage
Study Size (S:P) Statin Initiation Duration Vasospasm DCI Poor outcome Mortality
therapy
Randomized controlled trials
Tseng et al. [15] 80 (40:40) Pra 40 mg qd 72 h 14 days or 43% vs. 63% 5% vs. 30% 43% vs. 53% 5% vs. 20%
discharged (P = 0.006) (P < 0.001) (P = 0.7) (P = 0.04)
Lynch et al. [16] 39 (19:20) Sim 80 mg 48 h 14 days 26% vs. 60% 26% vs. 60% N/A N/A
qd (P = 0.03) (P = 0.03)
Chou et al. [17] 29 (19:20) Sim 80 mg 96 h 21 days 68% vs. 50% 37% vs. 50% 63% vs. 50% 0% vs. 15%
qd or ICU (P = 0.24) (P = 0.41) (P = 0.41) (P = 0.23)
discharged
Observational cohort study
Kramer et al. [21] 150 (71:79) Sim 80 mg Previously 14 days 42% vs. 41% 28% vs. 23% 28% in both N/A
qd (93%) used (P = 0.91) (P = 0.46) group
McGirt et al. [22] 340 (170:170) Sim 80 mg N/A 14 days 25.3% vs. 30.5% N/A 21.7% vs. 18.2% 18% vs. 15%
qd (P = 0.277) (P = 0.416) (P = 0.468)
Kern et al. [23] 135 (72:58) Pra 40 mg qd N/A 14 days 52% vs. 50% N/A 34.7% vs. 31.0% 20.8% vs. 13.7%
(P = 0.17) (P = 0.95) (P = 0.4)
Kern et al. [23] 100 (49:51) Sim 20, 40 N/A 14 days N/A 20% vs. 16% N/A 14% vs. 27%
mg qd (P = 0.74) (P = 0.20)
S:P: statin:placebo; Pra: pravastatin; Sim: simvastatin; qd: once a day; TCD: transcranial Doppler; DCI: delayed cerebral ischemia; N/A: not available; ICU: intensive
care unit; H: hours.
Figure 1: Flow chart of the literature selection for (a) subarachnoid hemorrhage, (b) intracerebral hemorrhage and (c) acute cerebral infarction.
RCTs: randomized controlled trials
independent beneficial pleiotropic effects, including primary and secondary stroke prevention. Promising
[5]
[6]
immunomodulation, [2] neuroprotection and cellular data has been published from studies of acute myocardial
[3]
senescence. These properties could be beneficial in infarction and casecontrolled studies of statin use
[7]
[4]
various acute neurologic diseases. prior to stroke led to an interest in determining the
[8]
role of statins in the acute setting, such asreducing early
Statins were initially developed for secondary prevention recurrence of ischemic event or beneficial for long-term
of cardiovascular disease via secondary to dyslipidemia. functional outcome.
Initial studies in neurological disease focused on patients
with stroke or at high risk of stroke. Long-term statin The aim of this review is to summarize the literature
therapy was associated with meaningful reductions in regarding the use of statins in common acute neurological
stroke, myocardial infarction and vascular death in both diseases; subarachnoid hemorrhage (SAH), intracerebral
134 Neuroimmunol Neuroinflammation | Volume 3 | June 20, 2016