Page 92 - Read Online
P. 92
Chiu Modified parasternal approach for aortic valve surgery
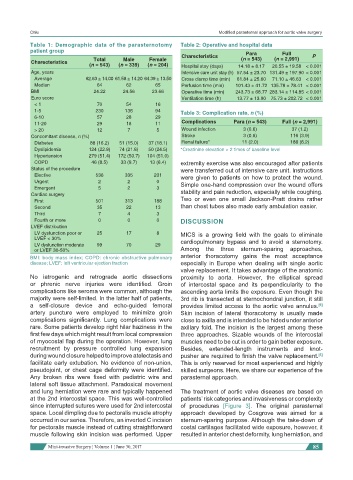
Table 1: Demographic data of the parasternotomy Table 2: Operative and hospital data
patient group
Charecteristics Para Full P
Charecteristics Total Male Female (n = 543) (n = 2,991)
(n = 543) (n = 339) (n = 204) Hospital stay (days) 14.18 ± 8.17 20.55 ± 19.58 < 0.001
Age, years Intensive care unit stay (h) 57.54 ± 23.70 131.49 ± 197.90 < 0.001
Average 62.63 ± 14.00 61.58 ± 14.20 64.39 ± 13.50 Cross clamp time (min) 61.84 ± 25.60 71.10 ± 46.63 < 0.001
Median 64 62 65 Perfusion time (min) 101.43 ± 41.72 135.78 ± 78.41 < 0.001
BMI 24.22 24.56 23.66 Operative time (min) 243.73 ± 68.77 283.14 ± 114.85 < 0.001
Euro score Ventilation time (h) 13.77 ± 13.90 75.73 ± 202.72 < 0.001
< 1 70 54 16
1-5 230 136 94 Table 3: Complication rate, n (%)
6-10 57 28 29
11-20 29 18 11 Complications Para (n = 543) Full (n = 2,991)
> 20 12 7 5 Wound infection 3 (0.6) 37 (1.2)
Concomitant disease, n (%) Stroke 3 (0.6) 116 (3.9)
Diabetes 88 (16.2) 51 (15.0) 37 (18.1) Renal failure* 11 (2.0) 186 (6.2)
Dyslipidemia 124 (22.8) 74 (21.8) 50 (24.5) *Creatinine elevation > 2 times of baseline level
Hypertension 279 (51.4) 172 (50.7) 104 (51.0)
COPD 46 (8.5) 33 (9.7) 13 (6.4) extremity exercise was also encouraged after patients
Status of the procedure were transferred out of intensive care unit. Instructions
Elective 536 335 201 were given to patients on how to protect the wound.
Urgent 2 2 0 Simple one-hand compression over the wound offers
Emergent 5 2 3
Cardiac surgery stability and pain reduction, especially while coughing.
First 501 313 188 Two or even one small Jackson-Pratt drains rather
Second 35 22 13 than chest tubes also made early ambulation easier.
Third 7 4 3
Fourth or more 0 0 0 DISCUSSION
LVEF distribution
LV dysfunction poor or 25 17 8 MICS is a growing field with the goals to eliminate
LVEF < 30% cardiopulmonary bypass and to avoid a sternotomy.
LV dysfunction moderate 99 70 29
or LVEF 30-50% Among the three sternum-sparing approaches,
BMI: body mass index; COPD: chronic obstructive pulmonary anterior thoracotomy gains the most acceptance
disease; LVEF: left ventricular ejection fraction especially in Europe when dealing with single aortic
valve replacement. It takes advantage of the anatomic
No iatrogenic and retrograde aortic dissections proximity to aorta. However, the elliptical spread
or phrenic nerve injuries were identified. Groin of intercostal space and its perpendicularity to the
complications like seroma were common, although the ascending aorta limits the exposure. Even though the
majority were self-limited. In the latter half of patients, 3rd rib is transected at sternochondral junction, it still
a self-closure device and echo-guided femoral provides limited access to the aortic valve annulus.
[9]
artery puncture were employed to minimize groin Skin incision of lateral thoracotomy is usually made
complications significantly. Lung complications were close to axilla and is intended to be hided under anterior
rare. Some patients develop right hilar haziness in the axillary fold. The incision is the largest among these
first few days which might result from local compression three approaches. Sizable wounds of the intercostal
of myocostal flap during the operation. However, lung muscles need to be cut in order to gain better exposure.
recruitment by pressure controlled lung expansion Besides, extended-length instruments and knot-
during wound closure helped to improve atelectasis and pusher are required to finish the valve replacement.
[5]
facilitate early extubation. No evidence of non-union, This is only reserved for most experienced and highly
pseudojoint, or chest cage deformity were identified. skilled surgeons. Here, we share our experience of the
Any broken ribs were fixed with pediatric wire and parasternal approach.
lateral soft tissue attachment. Paradoxical movement
and lung herniation were rare and typically happened The treatment of aortic valve diseases are based on
at the 2nd intercostal space. This was well-controlled patients’ risk categories and invasiveness or complexity
since interrupted sutures were used for 2nd intercostal of procedures [Figure 3]. The original parasternal
space. Local dimpling due to pectoralis muscle atrophy approach developed by Cosgrove was aimed for a
occurred in our series. Therefore, an inverted C incision sternum-sparing purpose. Although the take-down of
for pectoralis muscle instead of cutting straightforward costal cartilages facilitated wide exposure, however, it
muscle following skin incision was performed. Upper resulted in anterior chest deformity, lung herniation, and
Mini-invasive Surgery ¦ Volume 1 ¦ June 30, 2017 85