Page 183 - Read Online
P. 183
Isetani et al. Laparoscopic surgery for gallbladder carcinoma
deviation was 301 ± 102 min. dissection had an OT of 300, 442, and 488 min; BL
of 500, 200, and 143 mL; and LOS of 17, 34, and 24
The OT among the 79 patients in the PR group, 11 days, respectively. The third patient underwent the
in the LLS group, 25 in the AR group, and 9 in the surgery, 2 weeks after the first cholecystectomy of
SAR group was 245 (84-700) and 292 ± 140 min, 328 severe cholecystitis, for the T2 GBC revealed in the
(150-682) and 343 ± 152 min, 458 (224-848) and 504 postoperative pathological examination [Table 1].
± 161 min, and 352 (274-696) and 415 ± 159 min,
respectively. The other seven patients who underwent LLR of the
GB bed with peri-cystic LN and peri-bile duct LN
In the comparison of the OT between patients with dissections had an OT of 248 (186-340) and 254 ±
GBTs and patients in the other laparoscopic surgery 61 min, BL of 50 (10-250) and 91 ± 82 mL, and LOS of
groups (PR, LLS, AR, and SAR) a significant difference 11 (8-105) and 25 ± 35 days [Table 1].
was found between the GBT and AR groups [Table 2].
DISCUSSION
Intraoperative BL in each group
The BL in patients with GBTs was 109 (10-500) and Although no differences in LOS were observed, the
148 ± 145 mL. The BL in patients who underwent PR, BL and OT were significantly lower in the GBT than
LLS, AR, and SAR was 50 (0/uncountable-3,270) and AR group. Additionally, no differences were observed
278 ± 556 mL, 100 (10-516) and 166 ± 182 mL, 375 in the conversion, morbidity, or mortality rate between
(25-3,569) and 758 ± 911 mL, and 705 (35-1,920) and laparoscopic GBT surgery and conventional LLR
821 ± 794 mL, respectively. of any type. When compared with other types of
conventional LLR, the short-term results (OT, BL, and
In the comparison of BL between patients with GBTs LOS) of all 10 patients with GBTs were comparable
and patients in the other laparoscopic surgery groups with those in the LLS group. Three patients with T2
(PR, LLS, AR, and SAR), a significant difference was GBC who underwent LLR of S4b+5+6a with regional
found between the GBT and AR groups [Table 2]. LN dissection had perioperative short-term results
comparable with those of patients who underwent
Postoperative LOS in each group AR, although the number of patients was small.
The LOS in patients with GBTs was 16 (8-105) and The perioperative short-term results of the other
25 ± 29 days. The LOS in the PR, LLS, AR, and SAR 7 patients who underwent LLR of the GB bed with
groups was 15 (5-254) and 20 ± 30 days, 13 (11-52) peri-cystic duct LN and peri-bile duct LN dissections
and 19 ± 64 days, 22 (8-44) and 24 ± 12 days, and 15 were comparable even with those of patients who
(8-44) and 21 ± 15 days, respectively. underwent PR. LLR of the GB bed or S4b+5+6a with
LN dissection was feasible for treatment of GBTs of
No significant differences were found in the LOS the body/fundus suspected to be T1b/T2 GBC without
between patients with GBTs and patients in the other cystic duct invasion. Itano et al. reported that
[8]
laparoscopic surgery groups (PR, LLS, AR, and SAR) laparoscopic surgery for T2 GBC had a comparable
[Table 2]. OT (368 vs. 352 min), significantly smaller BL volume
(152 vs. 777 mL), shorter LOS (9.1 vs. 21.6 days),
Short-term results of LLR of S4b+5+6a (with and similar morbidity rate (1/15 vs. 3/11 patients)
regional LN dissection) and LLR of GB bed compared with open surgery. Our results are similar
(with peri-cystic LN and peri-bile duct LN to those from their laparoscopic surgeries. LLR has
dissection) the advantages of a smaller BL volume and shorter
Of the 10 patients with GBTs, 3 patients with T2 GBC LOS in some conditions, such as minor resections
who underwent LLR of S4b+5+6a with regional LN of the anterolateral segments. LLR of S4b+5+6a
[5]
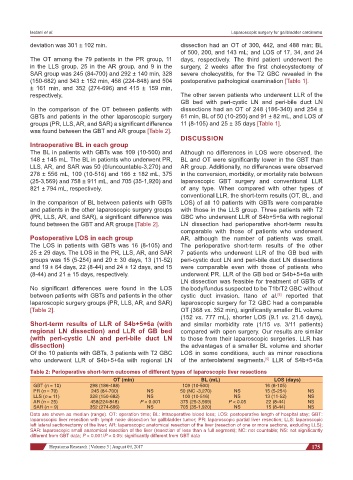
Table 2: Perioperative short-term outcomes of different types of laparoscopic liver resections
OT (min) BL (mL) LOS (days)
GBT (n = 10) 298 (186-488) 109 (10-500) 16 (8-105)
PR (n = 79) 245 (84-700) NS 50 (NC -3,270) NS 15 (5-254) NS
LLS (n = 11) 328 (150-682) NS 100 (10-516) NS 13 (11-52) NS
AR (n = 25) 458(224-848) P < 0.001 375 (25-3,569) P < 0.05 22 (8-44) NS
SAR (n = 9) 352 (274-696) NS 705 (35-1,920) NS 15 (8-44) NS
Data are shown as median (range). OT: operation time; BL: intraoperative blood loss; LOS: postoperative length of hospital stay; GBT:
laparoscopic liver resection with lymph node dissection for gallbladder tumor; PR: laparoscopic partial liver resection; LLS: laparoscopic
left lateral sectionectomy of the liver; AR: laparoscopic anatomical resection of the liver (resection of one or more sections, excluding LLS);
SAR: laparoscopic small anatomical resection of the liver (resection of less than a full segment); NC: not countable; NS: not significantly
different from GBT data; P < 0.001/P < 0.05: significantly different from GBT data
Hepatoma Research ¦ Volume 3 ¦ August 09, 2017 175