Page 182 - Read Online
P. 182
Isetani et al. Laparoscopic surgery for gallbladder carcinoma
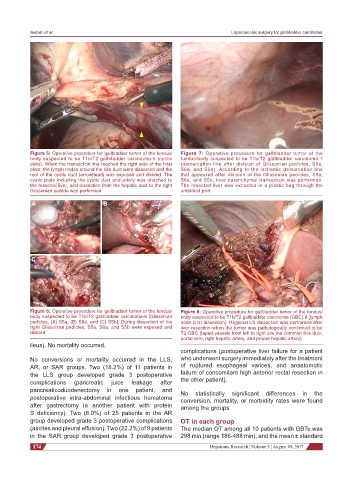
Figure 5: Operative procedure for gallbladder tumor of the fundus/ Figure 7: Operative procedure for gallbladder tumor of the
body suspected to be T1b/T2 gallbladder carcinoma-5 (cystic fundus/body suspected to be T1b/T2 gallbladder carcinoma-7
plate). When the transection line reached the right side of the hilar (demarcation line after division of Glissonian pedicles, S5a,
plate, the lymph nodes around the bile duct were dissected and the S6a, and S5b). According to the ischemic demarcation line
root of the cystic duct (arrowhead) was exposed and divided. The that appeared after division of the Glissonian pedicles, S5a,
cystic plate including the cystic duct and artery was attached to S6a, and S5b, liver parenchymal transection was performed.
the resected liver, and dissection from the hepatic duct to the right The resected liver was extracted in a plastic bag through the
Glissonian pedicle was performed umbilical port
A B
C
Figure 6: Operative procedure for gallbladder tumor of the fundus/ Figure 8: Operative procedure for gallbladder tumor of the fundus/
body suspected to be T1b/T2 gallbladder carcinoma-6 [Glissonian body suspected to be T1b/T2 gallbladder carcinoma (GBC)-8 [lymph
pedicles, (A) S5a, (B) S6a, and (C) S5b]. During dissection of the node (LN) dissection]. Regional LN dissection was performed after
right Glissonian pedicles, S5a, S6a, and S5b were exposed and liver resection when the tumor was pathologically confirmed to be
divided T2 GBC (taped vessels from left to right are the common bile duct,
portal vein, right hepatic artery, and proper hepatic artery)
ileus). No mortality occurred.
complications (postoperative liver failure for a patient
No conversions or mortality occurred in the LLS, who underwent surgery immediately after the treatment
AR, or SAR groups. Two (18.2%) of 11 patients in of ruptured esophageal varices, and anastomotic
the LLS group developed grade 3 postoperative failure of concomitant high anterior rectal resection in
complications (pancreatic juice leakage after the other patient).
pancreaticoduodenectomy in one patient, and No statistically significant differences in the
postoperative intra-abdominal infectious hematoma conversion, mortality, or morbidity rates were found
after gastrectomy in another patient with protein among the groups.
S deficiency). Two (8.0%) of 25 patients in the AR
group developed grade 3 postoperative complications OT in each group
(ascites and pleural effusion). Two (22.2%) of 9 patients The median OT among all 10 patients with GBTs was
in the SAR group developed grade 3 postoperative 298 min (range 186-488 min), and the mean ± standard
174 Hepatoma Research ¦ Volume 3 ¦ August 09, 2017