Page 51 - Read Online
P. 51
Shapey et al. Art Int Surg 2023;3:1-13 https://dx.doi.org/10.20517/ais.2022.31 Page 9
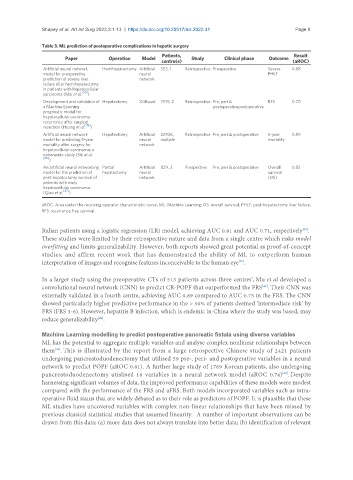
Table 3. ML prediction of postoperative complications in hepatic surgery
Patients, Result
Paper Operation Model Study Clinical phase Outcome
centre(s) (aROC)
Artificial neural network Hemihepatectomy Artificial 353, 1 Retrospective Preoperative Severe 0.88
model for preoperative neural PHLF
prediction of severe liver network
failure after hemihepatectomy
in patients with hepatocellular
[50]
carcinoma (Mai et al. )
Development and validation of Hepatectomy XGBoost 7919, 2 Retrospective Pre, peri & RFS 0.70
a Machine Learning postoperativepostoperative
prognostic model for
hepatocellular carcinoma
recurrence after surgical
[49]
resection (Huang et al. )
Artificial neural network Hepatectomy Artificial 22926, Retrospective Pre, peri & postoperative 5-year 0.89
model for predicting 5-year neural multiple mortality
mortality after surgery for network
hepatocellular carcinoma: a
nationwide study (Shi et al.
[46]
)
An artificial neural networking Partial Artificial 829, 2 Prospective Pre, peri & postoperative Overall 0.83
model for the prediction of hepatectomy neural survival
post-hepatectomy survival of network (OS)
patients with early
hepatocellular carcinoma
(Qiao et al. [47] )
aROC: Area under the receiving operator characteristic curve; ML: Machine Learning; OS: overall survival; PHLF: post-hepatectomy liver failure;
RFS: recurrence free survival.
Italian patients using a logistic regression (LR) model, achieving AUC 0.81 and AUC 0.71, respectively .
[39]
These studies were limited by their retrospective nature and data from a single centre which risks model
overfitting and limits generalizability. However, both reports showed great potential as proof-of-concept
studies, and affirm recent work that has demonstrated the ability of ML to outperform human
interpretation of images and recognise features inconceivable to the human eye .
[40]
7
In a larger study using the preoperative CTs of 513 patients across three centres , Mu et al developed a
convolutional neural network (CNN) to predict CR-POPF that outperformed the FRS . Their CNN was
[41]
externally validated in a fourth centre, achieving AUC 0.89 compared to AUC 0.73 in the FRS. The CNN
showed particularly higher predictive performance in the > 50% of patients deemed ‘intermediate risk’ by
FRS (FRS 3-6). However, hepatitis B infection, which is endemic in China where the study was based, may
[42]
reduce generalizability .
Machine Learning modelling to predict postoperative pancreatic fistula using diverse variables
ML has the potential to aggregate multiple variables and analyse complex nonlinear relationships between
them . This is illustrated by the report from a large retrospective Chinese study of 2421 patients
[43]
undergoing pancreatoduodenectomy that utilised 59 pre-, peri- and postoperative variables in a neural
network to predict POPF (aROC 0.81). A further large study of 1769 Korean patients, also undergoing
[44]
pancreatoduodenectomy utislised 16 variables in a neural network model (aROC 0.74) . Despite
harnessing significant volumes of data, the improved performance capabilities of these models were modest
compared with the performance of the FRS and aFRS. Both models incorporated variables such as intra-
operative fluid status that are widely debated as to their role as predictors of POPF. It is plausible that these
ML studies have uncovered variables with complex non-linear relationships that have been missed by
previous classical statistical studies that assumed linearity. A number of important observations can be
drawn from this data: (a) more data does not always translate into better data; (b) identification of relevant