Page 50 - Read Online
P. 50
Page 8 Shapey et al. Art Int Surg 2023;3:1-13 https://dx.doi.org/10.20517/ais.2022.31
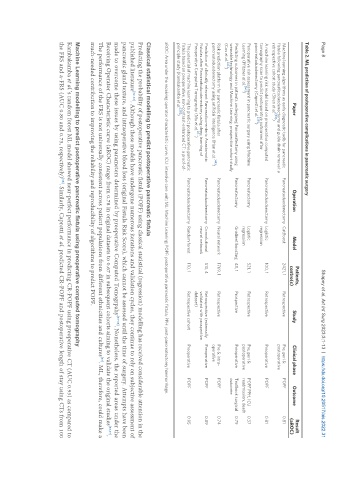
Table 2. ML prediction of postoperative complications in pancreatic surgery
Patients, Result
Paper Operation Model Study Clinical phase Outcome
centre(s) (aROC)
Machine learning algorithms as early diagnostic tools for pancreatic Pancreatoduodenectomy CatBoost 2421, 1 Retrospective Pre, peri & POPF 0.81
fistula following pancreaticoduodenectomy and guide drain removal: a postoperative
[53]
retrospective cohort study (Shen et al. )
A machine learning risk model based on preoperative computed Pancreatoduodenectomy Logistic 100, 1 Retrospective Preoperative POPF 0.81
tomography scan to predict postoperative outcomes after regression
[39]
pancreatoduodenectomy (Capretti et al. )
Perioperative risk assessment in pancreatic surgery using Machine Pancreatectomy Logistic 521, 1 Retrospective Pre, peri & POPF PPH, ICU 0.37
Learning (Pfitzner et al. [54] ) regression postoperative readmission, death
Predicting outcomes in patients undergoing Pancreatectomy using Pancreatectomy Gradient boosting 48, 1 Prospective Preoperative Textbook surgical 0.79
wearable technology and Machine Learning: prospective cohort study outcome
(Cos et al. [45] )
Risk prediction platform for pancreatic fistula after Pancreatoduodenectomy Neural network 1769, 1 Retrospective Pre & intra- POPF 0.74
pancreatoduodenectomy using artificial intelligence (Han et al. [44] ) operative
Prediction of clinically relevant Pancreatico-enteric Anastomotic Pancreatoduodenectomy Convolutional 513, 4 Retrospective (externally Preoperative POPF 0.89
Fistulas after Pancreatoduodenectomy using deep learning of neural network validated with prospective
[41]
Preoperative Computed Tomography (Mu et al. ) dataset)
The potential of machine learning to predict postoperative pancreatic Pancreatoduodenectomy Random forest 110, 1 Retrospective cohort Preoperative POPF 0.95
fistula based on preoperative, non-contrast-enhanced CT: a proof-of-
[38]
principle study (Kambakamba et al. )
aROC: Area under the receiving operator characteristic curve; ICU: intensive care unit; ML: Machine Learning; POPF: postoperative pancreatic fistula; PPH: post-pancreatectomy haemorrhage.
Classical statistical modelling to predict postoperative pancreatic fistula
Predicting the probability of postoperative pancreatic fistula (POPF) using classical statistical (regression) modelling has received considerable attention in the
published literature [32-35] . Although these models have undergone numerous iterations and validation cycles, they continue to rely on subjective assessment of
pancreatic gland texture, and intraoperative blood loss (original Fistula Risk Score), which cannot be assessed until the time of surgery. Attempts have been
made to overcome these issues by using parameters determined by preoperative Computed Tomogrpahy [35-36] . Nonetheless, the reported areas under the
Receiving Operator Characteristic curve (aROC) range from 0.78 in original datasets to 0.67 in subsequent cohorts aiming to validate the original studies [33,37] .
The performance of the FRS is not universally consistent across patient populations from different ethnicities and cultures . ML, therefore, could make a
[37]
much-needed contribution to improving the reliability and reproducibility of algorithms to predict POPF.
Machine Learning modelling to predict postoperative pancreatic fistula using preoperative computed tomography
Kambakamba et al.’s random forest ML model showed near-perfect performance in predicting CR-POPF using preoperative CT (AUC 0.95) as compared to
the FRS and a-FRS (AUC 0.80 and 0.73, respectively) . Similarly, Capretti et al. predicted CR-POPF and postoperative length of stay using CTs from 100
[38]