Page 275 - Read Online
P. 275
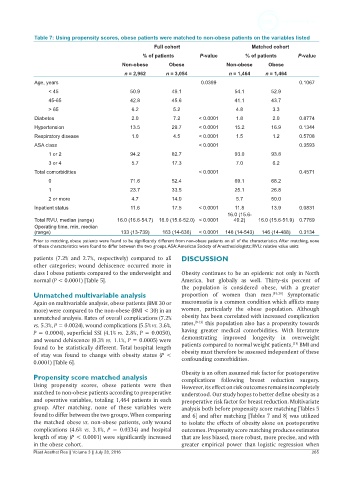
Table 7: Using propensity scores, obese patients were matched to non-obese patients on the variables listed
Full cohort Matched cohort
% of patients P-value % of patients P-value
Non-obese Obese Non-obese Obese
n = 2,962 n = 3,054 n = 1,464 n = 1,464
Age, years 0.0399 0.1067
< 45 50.9 49.1 54.1 52.9
45-65 42.8 45.6 41.1 43.7
> 65 6.2 5.2 4.8 3.3
Diabetes 2.0 7.2 < 0.0001 1.8 2.0 0.8774
Hypertension 13.5 29.7 < 0.0001 15.2 16.9 0.1344
Respiratory disease 1.0 4.5 < 0.0001 1.5 1.2 0.5708
ASA class < 0.0001 0.3593
1 or 2 94.2 82.7 93.0 93.8
3 or 4 5.7 17.3 7.0 6.2
Total comorbidities < 0.0001 0.4571
0 71.6 52.4 69.1 68.2
1 23.7 33.5 25.1 26.8
2 or more 4.7 14.0 5.7 50.0
Inpatient status 11.6 17.5 < 0.0001 11.8 13.9 0.0831
16.0 (15.6-
Total RVU, median (range) 16.0 (16.6-54.7) 16.0 (15.6-52.0) < 0.0001 49.2) 16.0 (15.6-51.9) 0.7769
Operating time, min, median
(range) 133 (13-739) 163 (14-636) < 0.0001 146 (14-543) 146 (14-488) 0.3134
Prior to matching, obese patients were found to be significantly different from non-obese patients on all of the characteristics. After matching, none
of these characteristics were found to differ between the two groups. ASA: American Society of Anesthesiologists; RVU: relative value units
patients (7.2% and 2.7%, respectively) compared to all DISCUSSION
other categories; wound dehiscence occurred more in
class I obese patients compared to the underweight and Obesity continues to be an epidemic not only in North
normal (P < 0.0001) [Table 5]. America, but globally as well. Thirty-six percent of
the population is considered obese, with a greater
Unmatched multivariable analysis proportion of women than men. [19,20] Symptomatic
Again on multivariable analysis, obese patients (BMI 30 or macromastia is a common condition which afflicts many
more) were compared to the non-obese (BMI < 30) in an women, particularly the obese population. Although
unmatched analysis. Rates of overall complications (7.2% obesity has been correlated with increased complication
vs. 5.3%, P = 0.0024), wound complications (5.5% vs. 3.6%, rates, [9-13] this population also has a propensity towards
P = 0.0004), superficial SSI (4.1% vs. 2.8%, P = 0.0050), having greater medical comorbidities. With literature
and wound dehiscence (0.3% vs. 1.1%, P = 0.0005) were demonstrating improved longevity in overweight
[21]
found to be statistically different. Total hospital length patients compared to normal weight patients, BMI and
of stay was found to change with obesity status (P < obesity must therefore be assessed independent of these
confounding comorbidities.
0.0001) [Table 6].
Obesity is an often assumed risk factor for postoperative
Propensity score matched analysis complications following breast reduction surgery.
Using propensity scores, obese patients were then However, its effect on risk outcomes remains incompletely
matched to non-obese patients according to preoperative understood. Our study hopes to better define obesity as a
and operative variables, totaling 1,464 patients in each preoperative risk factor for breast reduction. Multivariate
group. After matching, none of these variables were analysis both before propensity score matching [Tables 5
found to differ between the two groups. When comparing and 6] and after matching [Tables 7 and 8] was utilized
the matched obese vs. non-obese patients, only wound to isolate the effects of obesity alone on postoperative
complications (4.6% vs. 3.1%, P = 0.0334) and hospital outcomes. Propensity score matching produces estimates
length of stay (P < 0.0001) were significantly increased that are less biased, more robust, more precise, and with
in the obese cohort. greater empirical power than logistic regression when
Plast Aesthet Res || Volume 3 || July 28, 2016 265