Page 171 - Read Online
P. 171
Page 8 of 18 Avery et al. Mini-invasive Surg 2021;5:17 https://dx.doi.org/10.20517/2574-1225.2021.05
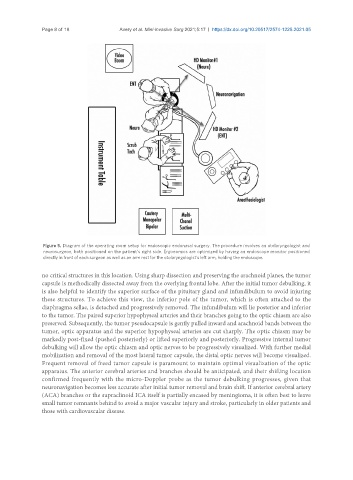
Figure 5. Diagram of the operating room setup for endoscopic endonasal surgery. The procedure involves an otolaryngologist and
neurosurgeon, both positioned on the patient’s right side. Ergonomics are optimized by having an endoscope monitor positioned
directly in front of each surgeon as well as an arm rest for the otolaryngologist’s left arm, holding the endoscope.
no critical structures in this location. Using sharp dissection and preserving the arachnoid planes, the tumor
capsule is methodically dissected away from the overlying frontal lobe. After the initial tumor debulking, it
is also helpful to identify the superior surface of the pituitary gland and infundibulum to avoid injuring
these structures. To achieve this view, the inferior pole of the tumor, which is often attached to the
diaphragma sellae, is detached and progressively removed. The infundibulum will lie posterior and inferior
to the tumor. The paired superior hypophyseal arteries and their branches going to the optic chiasm are also
preserved. Subsequently, the tumor pseudocapsule is gently pulled inward and arachnoid bands between the
tumor, optic apparatus and the superior hypophyseal arteries are cut sharply. The optic chiasm may be
markedly post-fixed (pushed posteriorly) or lifted superiorly and posteriorly. Progressive internal tumor
debulking will allow the optic chiasm and optic nerves to be progressively visualized. With further medial
mobilization and removal of the most lateral tumor capsule, the distal optic nerves will become visualized.
Frequent removal of freed tumor capsule is paramount to maintain optimal visualization of the optic
apparatus. The anterior cerebral arteries and branches should be anticipated, and their shifting location
confirmed frequently with the micro-Doppler probe as the tumor debulking progresses, given that
neuronavigation becomes less accurate after initial tumor removal and brain shift. If anterior cerebral artery
(ACA) branches or the supraclinoid ICA itself is partially encased by meningioma, it is often best to leave
small tumor remnants behind to avoid a major vascular injury and stroke, particularly in older patients and
those with cardiovascular disease.