Page 40 - Read Online
P. 40
Page 4 of 12 Na et al. Mini-invasive Surg 2024;8:31 https://dx.doi.org/10.20517/2574-1225.2024.10
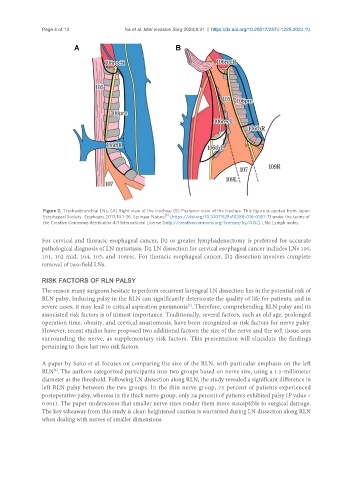
Figure 2. Tracheobronchial LNs. (A) Right view of the trachea; (B) Posterior view of the trachea. This figure is quoted from Japan
[6]
Esophageal Society. Esophagus. 2017;14:1-36. Springer Nature (https://doi.org/10.1007%2Fs10388-016-0551-7) under the terms of
the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/). LNs: Lymph nodes.
For cervical and thoracic esophageal cancer, D2 or greater lymphadenectomy is preferred for accurate
pathological diagnosis of LN metastasis. D2 LN dissection for cervical esophageal cancer includes LNs 100,
101, 102 mid, 104, 105, and 106rec. For thoracic esophageal cancer, D2 dissection involves complete
removal of two-field LNs.
RISK FACTORS OF RLN PALSY
The reason many surgeons hesitate to perform recurrent laryngeal LN dissection lies in the potential risk of
RLN palsy. Inducing palsy in the RLN can significantly deteriorate the quality of life for patients, and in
[7]
severe cases, it may lead to critical aspiration pneumonia . Therefore, comprehending RLN palsy and its
associated risk factors is of utmost importance. Traditionally, several factors, such as old age, prolonged
operation time, obesity, and cervical anastomosis, have been recognized as risk factors for nerve palsy.
However, recent studies have proposed two additional factors: the size of the nerve and the soft tissue area
surrounding the nerve, as supplementary risk factors. This presentation will elucidate the findings
pertaining to these last two risk factors.
A paper by Saito et al. focuses on comparing the size of the RLN, with particular emphasis on the left
RLN . The authors categorized participants into two groups based on nerve size, using a 1.5-millimeter
[8]
diameter as the threshold. Following LN dissection along RLN, the study revealed a significant difference in
left RLN palsy between the two groups. In the thin nerve group, 71 percent of patients experienced
postoperative palsy, whereas in the thick nerve group, only 24 percent of patients exhibited palsy (P value <
0.001). The paper underscores that smaller nerve sizes render them more susceptible to surgical damage.
The key takeaway from this study is clear: heightened caution is warranted during LN dissection along RLN
when dealing with nerves of smaller dimensions.