Page 42 - Read Online
P. 42
Page 6 of 12 Na et al. Mini-invasive Surg 2024;8:31 https://dx.doi.org/10.20517/2574-1225.2024.10
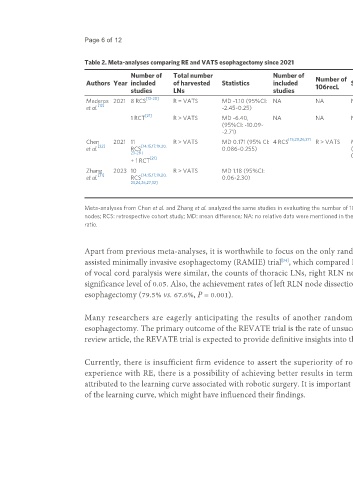
Table 2. Meta-analyses comparing RE and VATS esophagectomy since 2021
Number of Total number Number of Number of Number of Number of Palsy
Authors Year included of harvested Statistics included 106recL Statistics 106recR Statistics included rate Statistics
studies LNs studies studies
[13-20] [13-15,17,19,20]
Mederos 2021 8 RCS R = VATS MD -1.10 (95%CI: NA NA NA NA NA 6 RCS R = RD of 0.01 (95%CI:
[12]
et al. -2.45~0.25) VATS -0.08~0.10)
[21] [21]
1 RCT R > VATS MD -6.40, NA NA NA NA NA 1 RCT R = RD of -0.03 (95% CI:
(95%CI: -10.09~ VATS -0.11~0.05)
-2.71)
[15,20,26,27]
Chen 2021 11 R > VATS MD 0.171 (95% CI: 4 RCS R > VATS MD 0.219 R = VATS MD 0.10 13 R = RR 0.88 (95%CI:
[22] [14,15,17,19,20, [13,14,15,17,19,20,
et al. RCS 0.086~0.255) (95%CI: (95%CI: - RCS VATS 0.67~1.14)
23-28] 23,24,26-30]
[21] 0.097~0.340) 0.06~0.26) [21]
+ 1 RCT + 1 RCT
Zhang 2023 10 R > VATS MD 1.18 (95%CI: 11 R = R: 16.28% vs. VATS
[31] [14,15,17,19,20, [14,15,17,20,23,24,
et al. RCS 0.06~2.30) RCS VATS 21.96% (OR = 0.80;
23,24,26,27,32] 26,27,29,30,33]
[34] 95%CI: 0.57~1.12; P =
+ 1 RCT 0.19)
[22,31]
Meta-analyses from Chen et al. and Zhang et al. analyzed the same studies in evaluating the number of 106recL and 106recR . RE: Robotic esophagectomy; VATS: video-assisted thoracic surgery; LNs: lymph
nodes; RCS: retrospective cohort study; MD: mean difference; NA: no relative data were mentioned in the original articles; RD: risk difference; RCT: randomized controlled trial; RR: relative risk; R: robot; OR: odds
ratio.
Apart from previous meta-analyses, it is worthwhile to focus on the only randomized controlled study published in the English literature to date: the robot-
assisted minimally invasive esophagectomy (RAMIE) trial , which compared RE and VATS esophagectomy. While the number of dissected LNs and the rate
[34]
of vocal cord paralysis were similar, the counts of thoracic LNs, right RLN node, and left RLN node after neoadjuvant therapies were higher in RE, with a
significance level of 0.05. Also, the achievement rates of left RLN node dissection after neoadjuvant therapy were significantly higher in RE compared to VATS
esophagectomy (79.5% vs. 67.6%, P = 0.001).
Many researchers are eagerly anticipating the results of another randomized controlled trial, the REVATE trial , which compares RE and VATS
[35]
esophagectomy. The primary outcome of the REVATE trial is the rate of unsuccessful LN dissection along the left RLN. In relation to the subject matter of this
review article, the REVATE trial is expected to provide definitive insights into the left side.
Currently, there is insufficient firm evidence to assert the superiority of robotic surgery over VATS esophagectomy. However, as surgeons gain more
experience with RE, there is a possibility of achieving better results in terms of LN yield and lower rates of complications. This improvement could be
attributed to the learning curve associated with robotic surgery. It is important to note that some earlier studies may have included cases from the initial stages
of the learning curve, which might have influenced their findings.