Page 75 - Read Online
P. 75
McGivern et al. Art Int Surg 2023;3:27-47 https://dx.doi.org/10.20517/ais.2022.39 Page 33
by visual sensing technology surgery images
based on convolutional neural
network algorithm in the
diagnosis and treatment of
gallstones
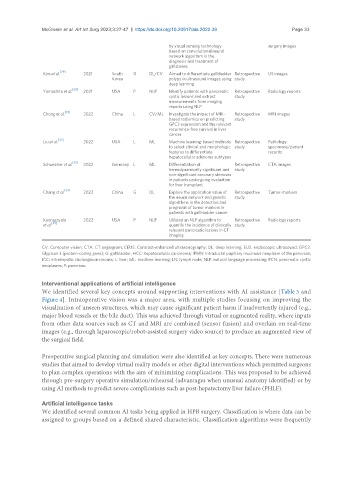
Kim et al. [29] 2021 South G DL/CV Aimed to differentiate gallbladder Retrospective US images
Korea polyps in ultrasound images using study
deep learning
[30]
Yamashita et al. 2021 USA P NLP Identify patients with pancreatic Retrospective Radiology reports
cystic lesions and extract study
measurements from imaging
reports using NLP
[31]
Chong et al. 2022 China L CV/ML Investigate the impact of MRI- Retrospective MRI images
based radiomics on predicting study
GPC3 expression and the relevant
recurrence-free survival in liver
cancer
[32]
Liu et al. 2022 USA L ML Machine learning-based methods Retrospective Pathology
to select clinical and morphologic study specimens/patient
features to differentiate records
hepatocellular adenoma subtypes
[33]
Schuessler et al. 2022 Germany L ML Differentiation of Retrospective CTA images
hemodynamically significant and study
non-significant coronary stenoses
in patients undergoing evaluation
for liver transplant
[34]
Chang et al. 2022 China G DL Explore the application value of Retrospective Tumor-markers
the neural network and genetic study
algorithms in the detection and
prognosis of tumor markers in
patients with gallbladder cancer
Kooragayala 2022 USA P NLP Utilized an NLP algorithm to Retrospective Radiology reports
[35]
et al. quantify the incidence of clinically study
relevant pancreatic lesions in CT
imaging
CV: Computer vision; CTA: CT angiogram; CEUS: Contrast-enhanced ultrasonography; DL: deep learning; EUS: endoscopic ultrasound; GPC3:
Glypican 3 (protein-coding gene); G: gallbladder; HCC: hepatocellular carcinoma; IPMN: Intraductal papillary mucinous neoplasm of the pancreas;
ICC: intrahepatic cholangiocarcinoma; L: liver; ML: machine learning; LN: lymph node; NLP: natural language processing; PCN: pancreatic cystic
neoplasms; P: pancreas.
Interventional applications of artificial intelligence
We identified several key concepts around supporting interventions with AI assistance [Table 3 and
Figure 4]. Intraoperative vision was a major area, with multiple studies focusing on improving the
visualization of unseen structures, which may cause significant patient harm if inadvertently injured (e.g.,
major blood vessels or the bile duct). This was achieved through virtual or augmented reality, where inputs
from other data sources such as CT and MRI are combined (sensor fusion) and overlain on real-time
images (e.g., through laparoscopic/robot-assisted surgery video source) to produce an augmented view of
the surgical field.
Preoperative surgical planning and simulation were also identified as key concepts. There were numerous
studies that aimed to develop virtual reality models or other digital interventions which permitted surgeons
to plan complex operations with the aim of minimizing complications. This was proposed to be achieved
through pre-surgery operative simulation/rehearsal (advantages when unusual anatomy identified) or by
using AI methods to predict severe complications such as post-hepatectomy liver failure (PHLF).
Artificial intelligence tasks
We identified several common AI tasks being applied in HPB surgery. Classification is where data can be
assigned to groups based on a defined shared characteristic. Classification algorithms were frequently