Page 15 - Read Online
P. 15
INTRODUCTION risks and outcomes associated with breast reconstruction
in underweight patients. We hypothesized that patients
Much has been published regarding the risks of obesity on who are at extremes of low BMI would have a higher risk of
medical outcomes. The prevalence of obesity among adults adverse outcomes.
in the United States has been steadily increasing over the
past several decades such that today over 1 in every 3 adults METHODS
is obese [body mass index (BMI) > 30 kg/m ], and nearly 1 in
2
every 10 adults is morbidly obese (BMI > 40 kg/m ). Obesity Patient population
2 [1,2]
is a multi-system disease process which confers increased
risk of medical comorbidities including hypertension All patients with “Plastics” recorded as their primary
(HTN), coronary artery disease, and diabetes mellitus (DM), surgical team were isolated from the 2006-2011 NSQIP
and increases the risk of surgical morbidity. [3,4] Similarly, database. Patients were stratified into either “prosthetic”
extremes of underweight have recently been described as a or “autologous” reconstruction cohorts, based on ACS-
risk factor for surgery. [5-7] Several recent studies of critically NSQIP classification. ACS-NSQIP tracks procedures based
and chronically ill patients, [8-11] and of patients undergoing on Current Procedural Terminology (CPT) codes. Specific
certain procedures [12-15] suggest that overweight and obese CPT codes used for each cohort include: 19340 (immediate
patients may paradoxically have better outcomes than breast reconstruction with implant), 19342 (delayed breast
underweight patients, given an increased risk for death and reconstruction with implant), 19357 (breast reconstruction
catastrophic complications in the latter patients. with tissue expander), 19361 (breast reconstruction with
latissimus dorsi flap), 19364 (breast reconstruction with
As many as 40% of women undergoing mastectomies in free flap), 19367 [breast reconstruction transverse rectus
the USA, they are now seeking post-mastectomy breast abdominis musculocutaneous (TRAM) flap] and 19368
reconstruction. [16-19] While much recent literature has (breast reconstruction with TRAM flap, with microvascular
detailed an association between obesity and poor surgical anastomosis). Patients undergoing multiple types of
outcomes, [20-23] other studies have failed to demonstrate reconstruction (e.g. latissimus dorsi flap + implant, or
an increased risk of death or severe complications in different types of reconstruction on each side) were
these patients. [24-26] Conversely, very little has been written excluded from analysis. Similarly, only patients with
about the risk of underweight patients undergoing breast total breast reconstruction using the above-mentioned
reconstruction. Such studies have been compromised by codes were included. Thus, patients undergoing breast
small sample sizes, single-institutional bias, retrospective reconstruction via fat grafting (CPT code 15770) or local flap
study design, limited patient follow-up, inconsistent closure (14301, 14302, 15734) were excluded from analysis.
definitions of underweight, types of surgical procedures Breast reconstruction patients were further categorized into
included, and outcomes studied. [27-30] prosthetic and autologous reconstruction cohorts. Similar
preoperative demographic and postoperative outcomes
In an effort to better understand the influence of BMI on analyses were carried out separately in the prosthetic and
outcomes following breast reconstruction, we examined autologous populations groups. Multivariate regression
the National Surgical Quality Improvement Program analysis was also conducted in similar fashion to the overall
(NSQIP) datasets. We aim to define and benchmark the population.
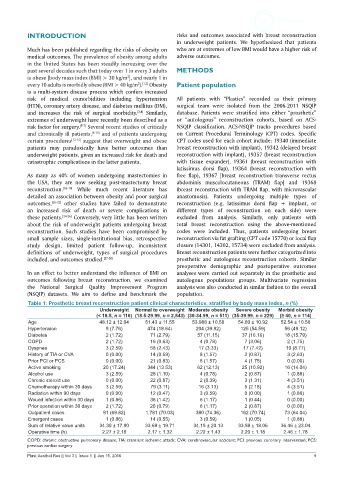
Table 1: Prosthetic breast reconstruction patient clinical characteristics, stratified by body mass index, n (%)
Underweight Normal to overweight Moderate obesity Severe obesity Morbid obesity
(< 18.5, n = 116) (18.5-29.99, n = 2,543) (30-34.99, n = 511) (35-39.99, n = 229) (≥ 40, n = 114)
Age 48.12 ± 12.04 51.43 ± 11.55 53.988 ± 10.58 54.60 ± 10.92 52.54 ± 10.56
Hypertension 9 (7.76) 474 (18.64) 204 (39.92) 125 (54.59) 56 (49.12)
Diabetes 2 (1.72) 71 (2.79) 57 (11.15) 37 (16.16) 18 (15.79)
COPD 2 (1.72) 16 (0.63) 4 (0.78) 7 (3.06) 2 (1.75)
Dyspnea 3 (2.59) 58 (2.43) 17 (3.33) 17 (7.42) 10 (8.77)
History of TIA or CVA 0 (0.00) 14 (0.59) 8 (1.57) 2 (0.87) 3 (2.63)
Prior PCI or PCS 0 (0.00) 21 (0.83) 8 (1.57) 4 (1.75) 0 (0.00)
Active smoking 20 (17.24) 344 (13.53) 62 (12.13) 25 (10.92) 16 (14.04)
Alcohol use 3 (2.59) 28 (1.10) 4 (0.78) 2 (0.87) 1 (0.88)
Chronic steroid use 0 (0.00) 22 (0.87) 2 (0.39) 3 (1.31) 4 (3.51)
Chemotherapy within 30 days 3 (2.59) 79 (3.11) 16 (3.13) 5 (2.18) 4 (3.51)
Radiation within 90 days 0 (0.00) 12 (0.47) 3 (0.59) 0 (0.00) 1 (0.88)
Wound infection within 30 days 1 (0.86) 36 (1.42) 6 (1.17) 1 (0.44) 0 (0.00)
Prior operation within 30 days 2 (1.72) 20 (0.79) 6 (1.17) 2 (0.87) 0 (0.00)
Outpatient cases 81 (69.82) 1,781 (70.03) 380 (74.36) 162 (70.74) 73 (64.04)
Emergent cases 1 (0.86) 14 (0.55) 3 (0.59) 1 (0.05) 1 (0.88)
Sum of relative value units 34.30 ± 17.90 33.69 ± 19.71 34.15 ± 20.13 33.59 ± 18.06 36.46 ± 23.04
Operative time (h) 2.27 ± 2.18 2.17 ± 1.32 2.22 ± 1.43 2.20 ± 1.18 2.46 ± 1.78
COPD: chronic obstructive pulmonary disease; TIA: transient ischemic attack; CVA: cerebrovascular accident; PCI: previous coronary intervention; PCS:
previous cardiac surgery
Plast Aesthet Res || Vol 3 || Issue 1 || Jan 15, 2016 9