Page 18 - Read Online
P. 18
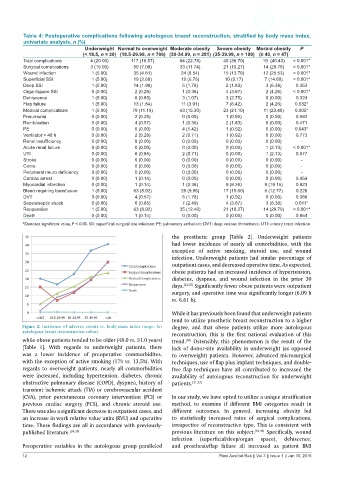
Table 4: Postoperative complications following autologous breast reconstruction, stratified by body mass index,
univariate analysis, n (%)
Underweight Normal to overweight Moderate obesity Severe obesity Morbid obesity P
(< 18.5, n = 20) (18.5-29.99, n = 706) (30-34.99, n = 281) (35-39.99, n = 109) (≥ 40, n = 47)
Total complications 4 (20.00) 117 (16.57) 64 (22.78) 40 (36.70) 19 (40.43) < 0.001*
Surgical complications 3 (15.00) 50 (7.08) 33 (11.74) 21 (19.27) 14 (29.79) < 0.001*
Wound infection 1 (5.00) 35 (4.61) 24 (8.54) 15 (13.76) 12 (25.53) < 0.001*
Superficial SSI 1 (5.00) 19 (2.69) 19 (6.76) 10 (9.17) 7 (14.89) < 0.001*
Deep SSI 1 (5.00) 14 (1.98) 5 (1.78) 2 (1.83) 3 (6.38) 0.353
Organ/space SSI 0 (0.00) 2 (0.28) 1 (0.36) 4 (3.67) 2 (4.26) < 0.001*
Dehiscence 1 (5.00) 6 (0.85) 3 (1.07) 3 (2.75) 0 (0.00) 0.324
Flap failure 1 (5.00) 13 (1.84) 11 (3.91) 7 (6.42) 2 (4.26) 0.032*
Medical complications 1 (5.00) 79 (11.19) 43 (15.30) 23 (21.10) 11 (23.40) 0.005*
Pneumonia 0 (0.00) 2 (0.28) 0 (0.00) 1 (0.92) 0 (0.00) 0.592
Reintubation 0 (0.00) 4 (0.57) 1 (0.36) 2 (1.83) 0 (0.00) 0.471
PE 0 (0.00) 0 (0.00) 4 (1.42) 1 (0.92) 0 (0.00) 0.043*
Ventilator > 48 h 0 (0.00) 2 (0.28) 2 (0.71) 1 (0.92) 0 (0.00) 0.773
Renal insufficiency 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) ‑
Acute renal failure 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) 1 (2.13) < 0.001*
UTI 0 (0.00) 6 (0.85) 2 (0.71) 0 (0.00) 1 (2.13) 0.677
Stroke 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) ‑
Coma 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) ‑
Peripheral neuro deficiency 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) 0 (0.00) ‑
Cardiac arrest 0 (0.00) 1 (0.14) 0 (0.00) 0 (0.00) 0 (0.00) 0.954
Myocardial infarction 0 (0.00) 1 (0.14) 1 (0.36) 9 (8.26) 9 (19.15) 0.923
Bleed requiring transfusion 1 (5.00) 63 (8.92) 28 (9.96) 17 (15.60) 6 (12.77) 0.226
DVT 0 (0.00) 4 (0.57) 5 (1.78) 1 (0.92) 0 (0.00) 0.388
Sepsis/septic shock 0 (0.00) 6 (0.85) 7 (2.49) 4 (3.67) 3 (6.38) 0.011*
Reoperation 1 (5.00) 63 (8.92) 35 (12.46) 21 (19.27) 14 (29.79) < 0.001*
Death 0 (0.00) 1 (0.14) 0 (0.00) 0 (0.00) 0 (0.00) 0.954
*Denotes significant value, P < 0.05. SSI: superficial surgical site infection; PE: pulmonary embolism; DVT: deep venous thrombosis; UTI: urinary tract infection
the prosthetic group [Table 2]. Underweight patients
had lower incidence of nearly all comorbidities, with the
exception of active smoking, steroid use, and wound
infection. Underweight patients had similar percentage of
outpatient cases, and decreased operative time. As expected,
obese patients had an increased incidence of hypertension,
diabetes, dyspnea, and wound infection in the prior 30
days. [24,25] Significantly fewer obese patients were outpatient
surgery, and operative time was significantly longer (6.09 h
vs. 6.61 h).
While it has previously been found that underweight patients
tend to utilize prosthetic breast reconstruction to a higher
Figure 2: Incidence of adverse events vs. body mass index range, for degree, and that obese patients utilize more autologous
autologous breast reconstruction cohort reconstruction, this is the first national evaluation of this
while obese patients tended to be older (48.0 vs. 51.0 years) trend. Ostensibly, this phenomenon is the result of the
[30]
[Table 1]. With regards to underweight patients, there lack of donor-site availability in underweight (as opposed
was a lower incidence of preoperative commorbidites, to overweight) patients. However, advanced microsurgical
with the exception of active smoking (17% vs. 13.5%). With techniques, use of flap plus implant techniques, and double-
regards to overweight patients, nearly all commorbidities free flap techniques have all contributed to increased the
were increased, including hypertension, diabetes, chronic availability of autologous reconstruction for underweight
obstructive pulmonary disease (COPD), dyspnea, history of patients. [31,32]
transient ischemic attack (TIA) or cerebrovascular accident
(CVA), prior percutaneous coronary intervention (PCI) or In our study, we have opted to utilize a unique stratification
previous cardiac surgery (PCS), and chronic steroid use. method, to examine if different BMI categories result in
There was also a significant decrease in outpatient cases, and different outcomes. In general, increasing obesity led
an increase in work relative value units (RVU) and operative to statistically increased rates of surgical complications,
time. These findings are all in accordance with previously- irrespective of reconstructive type. This is consistent with
published literature. [24,25] previous literature on this subject. [33,34] Specifically, wound
infection (superficial/deep/organ space), dehiscence,
Preoperative variables in the autologous group paralleled and prosthesis/flap failure all increased as patient BMI
12 Plast Aesthet Res || Vol 3 || Issue 1 || Jan 15, 2016