Page 16 - Read Online
P. 16
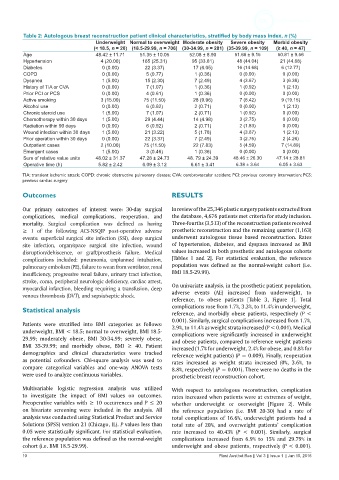
Table 2: Autologous breast reconstruction patient clinical characteristics, stratified by body mass index, n (%)
Underweight Normal to overweight Moderate obesity Severe obesity Morbid obesity
(< 18.5, n = 20) (18.5-29.99, n = 706) (30-34.99, n = 281) (35-39.99, n = 109) (≥ 40, n = 47)
Age 48.42 ± 11.71 51.35 ± 10.05 52.08 ± 8.90 51.66 ± 9.15 50.81 ± 9.56
Hypertension 4 (20.00) 165 (25.31) 95 (33.81) 48 (44.04) 21 (44.68)
Diabetes 0 (0.00) 22 (3.37) 17 (6.05) 16 (14.68) 6 (12.77)
COPD 0 (0.00) 5 (0.77) 1 (0.36) 0 (0.00) 0 (0.00)
Dyspnea 1 (5.00) 15 (2.30) 7 (2.49) 4 (3.67) 3 (6.38)
History of TIA or CVA 0 (0.00) 7 (1.07) 1 (0.36) 1 (0.92) 1 (2.13)
Prior PCI or PCS 0 (0.00) 4 (0.61) 1 (0.36) 0 (0.00) 0 (0.00)
Active smoking 3 (15.00) 75 (11.50) 28 (9.96) 7 (6.42) 9 (19.15)
Alcohol use 0 (0.00) 6 (0.92) 2 (0.71) 0 (0.00) 1 (2.13)
Chronic steroid use 1 (5.00) 7 (1.07) 2 (0.71) 1 (0.92) 0 (0.00)
Chemotherapy within 30 days 1 (5.00) 29 (4.44) 14 (4.98) 3 (2.75) 0 (0.00)
Radiation within 90 days 0 (0.00) 6 (0.92) 2 (0.71) 2 (1.83) 0 (0.00)
Wound infection within 30 days 1 (5.00) 21 (3.22) 5 (1.78) 4 (3.67) 1 (2.13)
Prior operation within 30 days 0 (0.00) 22 (3.37) 7 (2.49) 3 (2.75) 2 (4.26)
Outpatient cases 2 (10.00) 75 (11.50) 22 (7.83) 5 (4.59) 7 (14.89)
Emergent cases 1 (5.00) 3 (0.46) 1 (0.36) 0 (0.00) 0 (0.00)
Sum of relative value units 48.02 ± 31.37 47.28 ± 24.73 48. 79 ± 24.39 48.46 ± 26.30 47.14 ± 28.81
Operative time (h) 5.82 ± 2.42 6.09 ± 3.12 6.61 ± 3.41 6.38 ± 3.64 6.05 ± 3.63
TIA: transient ischemic attack; COPD: chronic obstructive pulmonary disease; CVA: cerebrovascular accident; PCI: previous coronary intervention; PCS:
previous cardiac surgery
Outcomes RESULTS
Our primary outcomes of interest were: 30-day surgical In review of the 25,346 plastic surgery patients extracted from
complications, medical complications, reoperation, and the database, 4,676 patients met criteria for study inclusion.
mortality. Surgical complication was defined as having Three-fourths (3,513) of the reconstruction patients received
≥ 1 of the following ACS-NSQIP post-operative adverse prosthetic reconstruction and the remaining quarter (1,163)
events: superficial surgical site infection (SSI), deep surgical underwent autologous tissue based reconstruction. Rates
site infection, organ/space surgical site infection, wound of hypertension, diabetes, and dyspnea increased as BMI
disruption/dehiscence, or graft/prosthesis failure. Medical values increased in both prosthetic and autologous cohorts
complications included: pneumonia, unplanned intubation, [Tables 1 and 2]. For statistical evaluation, the reference
pulmonary embolism (PE), failure to wean from ventilator, renal population was defined as the normal-weight cohort (i.e.
insufficiency, progressive renal failure, urinary tract infection, BMI 18.5-29.99).
stroke, coma, peripheral neurologic deficiency, cardiac arrest,
myocardial infarction, bleeding requiring a transfusion, deep On univariate analysis, in the prosthetic patient population,
venous thrombosis (DVT), and sepsis/septic shock. adverse events (AE) increased from underweight, to
reference, to obese patients [Table 3, Figure 1]. Total
complications rose from 1.7%, 3.3%, to 11.4% in underweight,
Statistical analysis
reference, and morbidly obese patients, respectively (P <
0.001). Similarly, surgical complications increased from 1.7%,
Patients were stratified into BMI categories as follows: 2.9%, to 11.4% as weight strata increased (P < 0.001). Medical
underweight, BMI < 18.5; normal to overweight, BMI 18.5- complications were significantly increased in underweight
29.99; moderately obese, BMI 30-34.99; severely obese, and obese patients, compared to reference weight patients
BMI 35-39.99; and morbidly obese, BMI ≥ 40. Patient increased (1.7% for underweight, 2.4% for obese, and 0.8% for
demographics and clinical characteristics were tracked reference weight patients) (P = 0.009). Finally, reoperation
as potential cofounders. Chi-square analysis was used to rates increased as weight strata increased (0%, 3.6%, to
compare categorical variables and one-way ANOVA tests 8.8%, respectively) (P = 0.001). There were no deaths in the
were used to analyze continuous variables. prosthetic breast reconstruction cohort.
Multivariable logistic regression analysis was utilized With respect to autologous reconstruction, complication
to investigate the impact of BMI values on outcomes. rates increased when patients were at extremes of weight,
Preoperative variables with ≥ 10 occurrences and P ≤ 20 whether underweight or overweight [Figure 2]. While
on bivariate screening were included in the analysis. All the reference population (i.e. BMI 20-30) had a rate of
analysis was conducted using Statistical Product and Service total complications of 16.6%, underweight patients had a
Solutions (SPSS) version 21 (Chicago, IL). P values less than total rate of 20%, and overweight patients’ complication
0.05 were statistically significant. For statistical evaluation, rate increased to 40.43% (P < 0.001). Similarly, surgical
the reference population was defined as the normal-weight complications increased from 6.9% to 15% and 29.79% in
cohort (i.e. BMI 18.5-29.99). underweight and obese patients, respectively (P < 0.001).
10 Plast Aesthet Res || Vol 3 || Issue 1 || Jan 15, 2016