Page 135 - Read Online
P. 135
Page 8 of 14 Foppiani et al. Plast Aesthet Res 2023;10:53 https://dx.doi.org/10.20517/2347-9264.2022.137
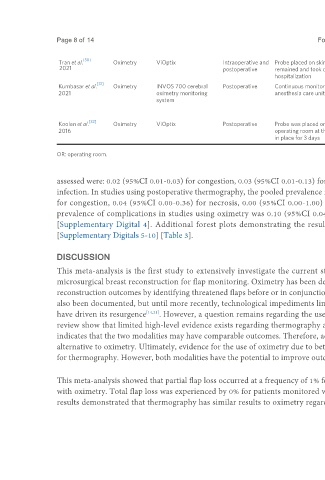
Tran et al. [30] Oximetry ViOptix Intraoperative and Probe placed on skin island intraoperatively after flap inset, A decrease in tissue saturation readings Until discharge (no
2021 postoperative remained and took continuous readings during the of 20 points from the postoperative mean length of stay
hospitalization baseline provided)
[31]
Kumbasar et al. Oximetry INVOS 700 cerebral Postoperative Continuous monitoring began postoperatively in the post- A 10% decrease in oximetry levels, 72 h
2021 oximetry monitoring anesthesia care unit and remained until discharge critical tissue oximetry measurements as
system a skeletal muscle oxygen saturation level
below 65%, or a drop in StO2 level of
more than 20% lasting for 20 minutes
[32]
Koolen et al. Oximetry ViOptix Postoperative Probe was placed onto the surface of the flap in the A rapid 20-point drop from baseline in 1 h 72 h
2016 operating room at the conclusion of the procedure and left or an absolute recording less than 30
in place for 3 days percent
OR: operating room.
assessed were: 0.02 (95%CI 0.01-0.03) for congestion, 0.03 (95%CI 0.01-0.13) for necrosis, 0.03 (95%CI 0.02-0.03) for hematoma and 0.01 (95%CI 0.00-0.16) for
infection. In studies using postoperative thermography, the pooled prevalence rates of the remaining flap complications assessed were: 0.03 (95%CI 0.00-0.29)
for congestion, 0.04 (95%CI 0.00-0.36) for necrosis, 0.00 (95%CI 0.00-1.00) for hematoma and 0.04 (95%CI 0.00-0.56) for infection. The overall pooled
prevalence of complications in studies using oximetry was 0.10 (95%CI 0.04-0.21) compared to 0.12 (95%CI 0.01-0.54) for those using thermography
[Supplementary Digital 4]. Additional forest plots demonstrating the results of this meta-analysis are available in the supplemental materials section
[Supplementary Digitals 5-10] [Table 3].
DISCUSSION
This meta-analysis is the first study to extensively investigate the current state of literature comparing the use of thermography to oximetry following
microsurgical breast reconstruction for flap monitoring. Oximetry has been described thoroughly in the literature and has significantly contributed to breast
reconstruction outcomes by identifying threatened flaps before or in conjunction with physical examination findings . Thermography for flap monitoring has
[14]
also been documented, but until more recently, technological impediments limited its use . In recent years, advances in smartphones and portable cameras
[14]
have driven its resurgence [14,21] . However, a question remains regarding the usefulness of thermography compared to oximetry. The results of this systematic
review show that limited high-level evidence exists regarding thermography as opposed to oximetry. The evidence that is available regarding each method
indicates that the two modalities may have comparable outcomes. Therefore, additional investigation could show the utility of thermography as an adjunct or
alternative to oximetry. Ultimately, evidence for the use of oximetry due to better salvage rate and lower overall complication rates may be stronger than that
for thermography. However, both modalities have the potential to improve outcomes, especially given additional research and development.
This meta-analysis showed that partial flap loss occurred at a frequency of 1% for patients monitored with thermography compared to 1% for those monitored
with oximetry. Total flap loss was experienced by 0% for patients monitored with thermography compared to 0% for those monitored with oximetry. These
results demonstrated that thermography has similar results to oximetry regarding partial and total flap loss. This emphasizes that both types of monitoring