Page 60 - Read Online
P. 60
Riachi et al. Mini-invasive Surg 2023;7:14 https://dx.doi.org/10.20517/2574-1225.2022.120 Page 5 of 11
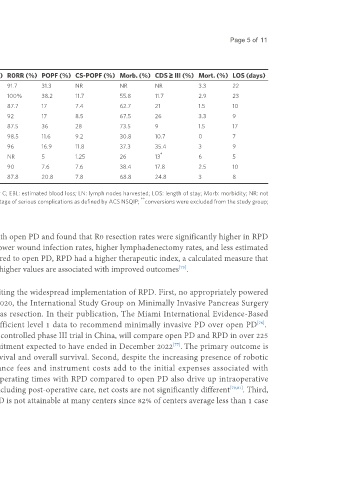
Table 1. Surgical and oncologic outcomes of RPD
Author N EBL (mean in ml) OR time (mean in minutes) Con. (%) LN (mean) R0RR (%) POPF (%) CS-POPF (%) Morb. (%) CDS ≥ III (%) Mort. (%) LOS (days)
[44]
Giulianotti et al. 60 394 421 18.3 18.7 91.7 31.3 NR NR NR 3.3 22
Boggi et al. [48] 34 220 597 0 32 100% 38.2 11.7 55.8 11.7 2.9 23
[45]
Zureikat et al. 132 300 527 8 19 87.7 17 7.4 62.7 21 1.5 10
[46]
Boone et al. 200 250 483 6.5 22 92 17 8.5 67.5 26 3.3 9
[49]
Boggi et al. 83 NR 527 1.5 37 87.5 36 28 73.5 9 1.5 17
[50]
Takahashi et al. 65 150 498 3 17 98.5 11.6 9.2 30.8 10.7 0 7
[51]
Guerra et al. 59 150 515 18.6 26 96 16.9 11.8 37.3 35.4 3 9
[52] *
Rosemurgy et al. 155 200 423 17 NR NR 5 1.25 26 13 6 5
[53] ** **
Valle et al. 39 200 477 15.2 23 90 7.6 7.6 38.4 17.8 2.5 10
[47]
Zureikat et al. 500 363 415 5.2 28 87.8 20.8 7.8 68.8 24.8 3 8
CDS: Clavien dindo score; Con.: conversion to OPD; CS-POPF: clinically significant POPF, i.e., Grade B or C; EBL: estimated blood loss; LN: lymph nodes harvested; LOS: length of stay; Morb: morbidity; NR: not
*
**
reported; N: number of patients that underwent RPD; OR: operating room; R0RR: R0 resection rate; percentage of serious complications as defined by ACS NSQIP; conversions were excluded from the study group;
the rest of the values are relative to the 39 remaining RPD patients.
analysis by Dong et al. focused on oncological outcomes in comparing RPD with open PD and found that R0 resection rates were significantly higher in RPD
with non-inferior overall survival outcomes. In addition, RPD demonstrated lower wound infection rates, higher lymphadenectomy rates, and less estimated
[74]
blood loss . Furthermore, a review by Mantzavinou et al. showed that, compared to open PD, RPD had a higher therapeutic index, a calculated measure that
includes lymphadenectomy rate, R0 resection rate, and 30-day mortality where higher values are associated with improved outcomes .
[75]
While the available evidence supports RPD utilization, challenges persist, limiting the widespread implementation of RPD. First, no appropriately powered
randomized controlled trial exists directly comparing RPD to open PD. In 2020, the International Study Group on Minimally Invasive Pancreas Surgery
published the first evidence-based guidelines on minimally invasive pancreas resection. In their publication, The Miami International Evidence-Based
Guidelines on Minimally Invasive Pancreas Resection, the authors cite insufficient level 1 data to recommend minimally invasive PD over open PD .
[76]
However, the PORTAL trial, an active multicenter non-inferiority randomized controlled phase III trial in China, will compare open PD and RPD in over 225
patients with benign, premalignant, and malignant disease, with patient recruitment expected to have ended in December 2022 . The primary outcome is
[77]
time to functional recovery with secondary outcomes of recurrence-free survival and overall survival. Second, despite the increasing presence of robotic
surgery over the last two decades, costs remain high. Recurring maintenance fees and instrument costs add to the initial expenses associated with
implementing a robotic surgery program . Furthermore, generally longer operating times with RPD compared to open PD also drive up intraoperative
[78]
costs [79,80] . However, after factoring in costs across a patient’s totality of care, including post-operative care, net costs are not significantly different [79,81] . Third,
the threshold of procedures needed to develop and maintain proficiency in RPD is not attainable at many centers since 82% of centers average less than 1 case