Page 99 - Read Online
P. 99
likely to benefi t from chemotherapy with a prolonged life
expectancy. Previous publications have suggested various
prognostic factors involved in advanced NSCLC using
heterogeneous patient populations. [12-15] In a recent study,
245 patients were analyzed with the aim of evaluating
factors associated with long-term survival (> 2 years) in
patients with advanced NSCLC. Fifty-two patients (21%)
had SCC. Six prognostic factors were identifi ed: PS of 0-1
at fi rst tumor progression, normal lactate dehydrogenase
levels at diagnosis, use of maintenance therapy, surgical
resection, time to progression of > 3 months, and
number of chemotherapy agents received. Conversely,
[13]
our study showed that a better PS at diagnosis was
signifi cantly associated with a better OS. In another large
[15]
report, FLEX investigated the prognostic signifi cance
of baseline characteristics and showed that age, gender,
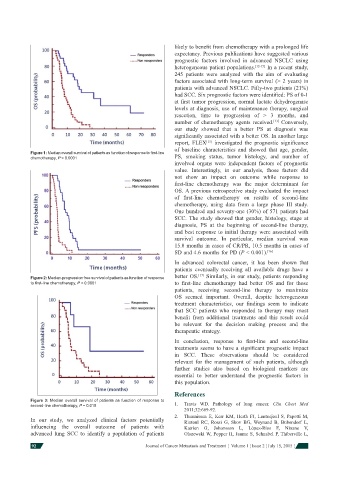
Figure 1: Median overall survival of patients as function of response to fi rst-line
chemotherapy, P < 0.0001 PS, smoking status, tumor histology, and number of
involved organs were independent factors of prognostic
value. Interestingly, in our analysis, those factors did
not show an impact on outcome while response to
fi rst-line chemotherapy was the major determinant for
OS. A previous retrospective study evaluated the impact
of fi rst-line chemotherapy on results of second-line
chemotherapy, using data from a large phase III study.
One hundred and seventy-one (30%) of 571 patients had
SCC. The study showed that gender, histology, stage at
diagnosis, PS at the beginning of second-line therapy,
and best response to initial therapy were associated with
survival outcome. In particular, median survival was
15.8 months in cases of CR/PR, 10.5 months in cases of
SD and 4.6 months for PD (P < 0.001). [16]
In advanced colorectal cancer, it has been shown that
patients eventually receiving all available drugs have a
[17]
Figure 2: Median-progression free survival of patients as function of response better OS. Similarly, in our study, patients responding
to fi rst-line chemotherapy, P < 0.0001 to fi rst-line chemotherapy had better OS and for those
patients, receiving second-line therapy to maximize
OS seemed important. Overall, despite heterogeneous
treatment characteristics, our fi ndings seem to indicate
that SCC patients who responded to therapy may most
benefi t from additional treatments and this result could
be relevant for the decision making process and the
therapeutic strategy.
In conclusion, response to fi rst-line and second-line
treatments seems to have a signifi cant prognostic impact
in SCC. These observations should be considered
relevant for the management of such patients, although
further studies also based on biological markers are
essential to better understand the prognostic factors in
this population.
References
Figure 3: Median overall survival of patients as function of response to
second-line chemotherapy, P = 0.015 1. Travis WD. Pathology of lung cancer. Clin Chest Med
2011;32:669-92.
2. Thunnissen E, Kerr KM, Herth FJ, Lantuejoul S, Papotti M,
In our study, we analyzed clinical factors potentially Rintoul RC, Rossi G, Skov BG, Weynand B, Bubendorf L,
infl uencing the overall outcome of patients with Katrien G, Johansson L, López-Ríos F, Ninane V,
advanced lung SCC to identify a population of patients Olszewski W, Popper H, Jaume S, Schnabel P, Thiberville L,
92 Journal of Cancer Metastasis and Treatment ¦ Volume 1 ¦ Issue 2 ¦ July 15, 2015 ¦