Page 13 - Read Online
P. 13
de Santis et al. Hepatoma Res 2019;5:1 I http://dx.doi.org/10.20517/2394-5079.2018.65 Page 5 of 16
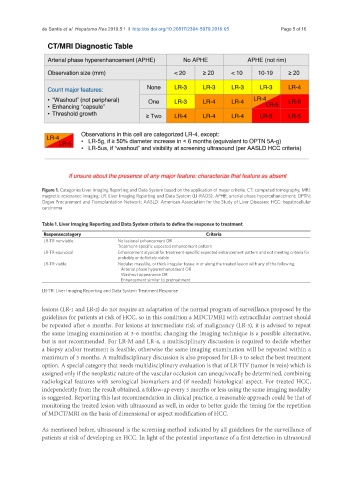
Figure 1. Categories Liver Imaging Reporting and Data System based on the application of major criteria. CT: computed tomography; MRI:
magnetic resonance imaging; LR: Liver Imaging Reporting and Data System (LI-RADS); APHE: arterial phase hyperenhancement; OPTN:
Organ Procurement and Transplantation Network; AASLD: American Association for the Study of Liver Diseases; HCC: hepatocellular
carcinoma
Table 1. Liver Imaging Reporting and Data System criteria to define the response to treatment
Responsecategory Criteria
LR-TR nonviable No lesional enhancement OR
Treatment-specific expected enhancement pattern
LR-TR equivocal Enhancement atypical for treatment-specific expected enhancement pattern and not meeting criteria for
probably or definitely viable
LR-TR viable Nodular, masslike, or thick irregular tissue in or along the treated lesion with any of the following:
Arterial phase hyperenhancement OR
Washout appearance OR
Enhancement similar to pretreatment
LR-TR: Liver Imaging Reporting and Data System Treatment Response
lesions (LR-1 and LR-2) do not require an adaptation of the normal program of surveillance proposed by the
guidelines for patients at risk of HCC, so in this condition a MDCT/MRI with extracellular contrast should
be repeated after 6 months. For lesions at intermediate risk of malignancy (LR-3), it is advised to repeat
the same imaging examination at 3-6 months; changing the imaging technique is a possible alternative,
but is not recommended. For LR-M and LR-4, a multisciplinary discussion is required to decide whether
a biopsy and/or treatment is feasible, otherwise the same imaging examination will be repeated within a
maximum of 3 months. A multidisciplinary discussion is also proposed for LR-5 to select the best treatment
option. A special category that needs multidisciplinary evaluation is that of LR-TIV (tumor in vein) which is
assigned only if the neoplastic nature of the vascular occlusion can unequivocally be determined, combining
radiological features with serological biomarkers and (if needed) histological aspect. For treated HCC,
independently from the result obtained, a follow-up every 3 months or less using the same imaging modality
is suggested. Reporting this last recommendation in clinical practice, a reasonable approach could be that of
monitoring the treated lesion with ultrasound as well, in order to better guide the timing for the repetition
of MDCT/MRI on the basis of dimensional or aspect modification of HCC.
As mentioned before, ultrasound is the screening method indicated by all guidelines for the surveillance of
patients at risk of developing an HCC. In light of the potential importance of a first detection in ultrasound