Page 148 - Read Online
P. 148
Tsutsui et al. Hepatoma Res 2018;4:13 I http://dx.doi.org/10.20517/2394-5079.2018.20 Page 9 of 11
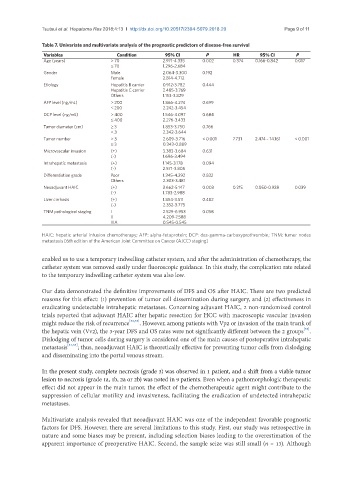
Table 7. Univariate and multivariate analysis of the prognostic predictors of disease-free survival
Variables Condition 95% CI P HR 95% CI P
Age (years) > 70 2.971-4.335 0.002 0.374 0.166-0.842 0.017
≤ 70 1.296-2.684
Gender Male 2.064-3.300 0.192
Female 2.814-4.712
Etiology Hepatitis B carrier 0.912-3.782 0.444
Hepatitis C carrier 2.485-3.769
Others 1.153-3.829
AFP level (ng/mL) > 200 1.866-4.274 0.699
≤ 200 2.242-3.454
DCP level (ng/mL) > 400 1.546-4.097 0.684
≤ 400 2.276-3.433
Tumor diameter (cm) ≥ 3 1.853-3.750 0.766
< 3 2.342-3.644
Tumor number > 3 2.609-3.716 < 0.001 7.731 2.474 – 14.161 < 0.001
≤ 3 0.343-0.889
Microvascular invasion (+) 3.383-3.684 0.631
(-) 1.696-3.494
Intrahepatic metastasis (+) 1.145-3.178 0.094
(-) 2.571-3.805
Differentiation grade Poor 1.345-4.292 0.832
Others 2.303-3.481
Neoadjuvant HAIC (+) 3.662-5.147 0.003 0.215 0.050-0.928 0.039
(-) 1.783-2.988
Liver cirrhosis (+) 1.854-3.511 0.482
(-) 2.352-3.775
TNM pathological staging I 2.529-6.953 0.058
II 4.209-7.588
IIIA 0.545-0.545
HAIC: hepatic arterial infusion chemotherapy; AFP: alpha-fetoprotein; DCP: des-gamma-carboxyprothrombin; TNM: tumor nodes
metastasis [6th edition of the American Joint Committee on Cancer (AJCC) staging]
enabled us to use a temporary indwelling catheter system, and after the administration of chemotherapy, the
catheter system was removed easily under fluoroscopic guidance. In this study, the complication rate related
to the temporary indwelling catheter system was also low.
Our data demonstrated the definitive improvements of DFS and OS after HAIC. There are two predicted
reasons for this effect: (1) prevention of tumor cell dissemination during surgery, and (2) effectiveness in
eradicating undetectable intrahepatic metastases. Concerning adjuvant HAIC, 2 non-randomized control
trials reported that adjuvant HAIC after hepatic resection for HCC with macroscopic vascular invasion
might reduce the risk of recurrence [32,33] . However, among patients with Vp2 or invasion of the main trunk of
[33]
the hepatic vein (Vv2), the 3-year DFS and OS rates were not significantly different between the 2 groups .
Dislodging of tumor cells during surgery is considered one of the main causes of postoperative intrahepatic
metastasis [34,35] ; thus, neoadjuvant HAIC is theoretically effective for preventing tumor cells from dislodging
and disseminating into the portal venous stream.
In the present study, complete necrosis (grade 3) was observed in 1 patient, and a shift from a viable tumor
lesion to necrosis (grade 1a, 1b, 2a or 2b) was noted in 9 patients. Even when a pathomorphologic therapeutic
effect did not appear in the main tumor, the effect of the chemotherapeutic agent might contribute to the
suppression of cellular motility and invasiveness, facilitating the eradication of undetected intrahepatic
metastases.
Multivariate analysis revealed that neoadjuvant HAIC was one of the independent favorable prognostic
factors for DFS. However, there are several limitations to this study. First, our study was retrospective in
nature and some biases may be present, including selection biases leading to the overestimation of the
apparent importance of preoperative HAIC. Second, the sample seize was still small (n = 13). Although