Page 305 - Read Online
P. 305
Cervantes-Gracia et al. Vessel Plus 2020;4:27 I http://dx.doi.org/10.20517/2574-1209.2020.22 Page 3 of 19
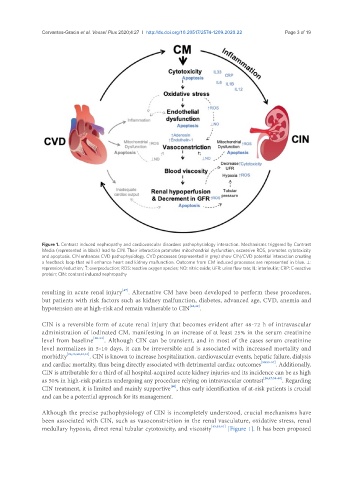
Figure 1. Contrast induced nephropathy and cardiovascular disorders pathophysiology interaction. Mechanisms triggered by Contrast
Media (represented in black) lead to CIN. Their interaction promotes mitochondrial dysfunction, excessive ROS, promotes cytotoxicity
and apoptosis. CIN enhances CVD pathophysiology. CVD processes (represented in grey) show CIN/CVD potential interaction creating
a feedback loop that will enhance heart and kidney malfunction. Outcome from CM induced processes are represented in blue. ⊥:
repression/reduction; ↑: overproduction; ROS: reactive oxygen species; NO: nitric oxide; UFR: urine flow rate; IL: interleukin; CRP: C-reactive
protein; CIN: contrast induced nephropathy
[47]
resulting in acute renal injury . Alternative CM have been developed to perform these procedures,
but patients with risk factors such as kidney malfunction, diabetes, advanced age, CVD, anemia and
hypotension are at high-risk and remain vulnerable to CIN [48,49] .
CIN is a reversible form of acute renal injury that becomes evident after 48-72 h of intravascular
administration of iodinated CM, manifesting in an increase of at least 25% in the serum creatinine
level from baseline [50-52] . Although CIN can be transient, and in most of the cases serum creatinine
level normalizes in 5-10 days, it can be irreversible and is associated with increased mortality and
morbidity [25,45,50,53,54] . CIN is known to increase hospitalization, cardiovascular events, hepatic failure, dialysis
and cardiac mortality, thus being directly associated with detrimental cardiac outcomes [50,55-57] . Additionally,
CIN is attributable for a third of all hospital-acquired acute kidney injuries and its incidence can be as high
as 50% in high-risk patients undergoing any procedure relying on intravascular contrast [26,47,58-60] . Regarding
[60]
CIN treatment, it is limited and mainly supportive , thus early identification of at-risk patients is crucial
and can be a potential approach for its management.
Although the precise pathophysiology of CIN is incompletely understood, crucial mechanisms have
been associated with CIN, such as vasoconstriction in the renal vasculature, oxidative stress, renal
medullary hypoxia, direct renal tubular cytotoxicity, and viscosity [45,53,61] [Figure 1]. It has been proposed