Page 320 - Read Online
P. 320
Echeverria-Villalobos et al. Vessel Plus 2019;3:33 I http://dx.doi.org/10.20517/2574-1209.2019.12 Page 3 of 12
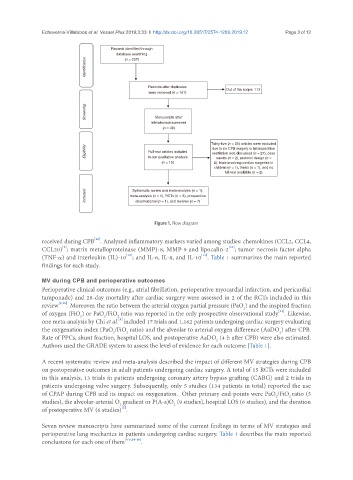
Records identified through
database searching
Identification
(n = 207)
Records after duplicates Out of the scope: 113
were removed (n = 161)
Screening Manuscripts after
title/abstract screened
(n = 48)
Thirty-five (n = 35) articles were excluded
Eligibility Full-text articles included due to no CPB surgery or intraoperative
ventilation was discussed (n = 27), case
in our qualitative analysis
reports (n = 2), protocol design (n =
(n = 13) 2), trials involving cardiac surgeries in
children (n = 1), thesis (n = 1), and no
full-text available (n = 2)
Included meta-analysis (n = 1), RCTs (n = 3), prospective
Systematic review and meta-analysis (n = 1),
observational (n = 1), and reviews (n = 7)
Figure 1. Flow diagram
[12]
received during CPB . Analyzed inflammatory markers varied among studies: chemokines (CCL2, CCL4,
[9]
[10]
CCL20) ; matrix metalloproteinase (MMP)-8, MMP-9 and lipocalin-2 ; tumor necrosis factor alpha
[12]
[11]
(TNF-α) and interleukin (IL)-10 ; and IL-6, IL-8, and IL-10 . Table 1 summarizes the main reported
findings for each study.
MV during CPB and perioperative outcomes
Perioperative clinical outcomes (e.g., atrial fibrillation, perioperative myocardial infarction, and pericardial
tamponade) and 28-day mortality after cardiac surgery were assessed in 2 of the RCTs included in this
review [9,10] . Moreover, the ratio between the arterial oxygen partial pressure (PaO ) and the inspired fraction
2
[12]
of oxygen (FiO ) or PaO /FiO ratio was reported in the only prospective observational study . Likewise,
2
2
2
[8]
one meta-analysis by Chi et al. included 17 trials and 1,162 patients undergoing cardiac surgery evaluating
the oxygenation index (PaO /FiO ratio) and the alveolar to arterial oxygen difference (AaDO ) after CPB.
2
2
2
Rate of PPCs, shunt fraction, hospital LOS, and postoperative AaDO (4 h after CPB) were also estimated.
2
Authors used the GRADE system to assess the level of evidence for each outcome [Table 1].
A recent systematic review and meta-analysis described the impact of different MV strategies during CPB
on postoperative outcomes in adult patients undergoing cardiac surgery. A total of 15 RCTs were included
in this analysis, 13 trials in patients undergoing coronary artery bypass grafting (CABG) and 2 trials in
patients undergoing valve surgery. Subsequently, only 5 studies (134 patients in total) reported the use
of CPAP during CPB and its impact on oxygenation. Other primary end-points were PaO /FiO ratio (5
2
2
studies), the alveolar-arterial O gradient or P(A-a)O (9 studies), hospital LOS (6 studies), and the duration
2
2
[2]
of postoperative MV (6 studies) .
Seven review manuscripts have summarized some of the current findings in terms of MV strategies and
perioperative lung mechanics in patients undergoing cardiac surgery. Table 1 describes the main reported
conclusions for each one of them [4-6,14-16] .