Page 125 - Read Online
P. 125
Zahrai et al. Vessel Plus 2023;7:32 https://dx.doi.org/10.20517/2574-1209.2023.100 Page 7 of 13
CABG groups was 1.91 (95% CI: 1.11-
3.29). This was 2.84 (1.31-6.14) for
undefined STEMI/NSTEMI and 0.96
(0.62-1.48) for the NSTEMI groups
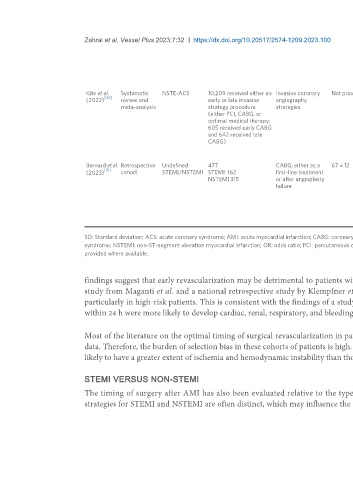
Kite et al. Systematic NSTE-ACS 10,209 received either an Invasive coronary Not provided Cut-off times for early and late All-cause mortality No significant differences were
[46]
(2022) review and early or late invasive angiography procedures were not defined by observed in the risk of all-cause
meta-analysis strategy procedure strategies authors. Authors extracted this mortality (risk ratio = 0.90, 95% CI
(either PCI, CABG, or data for each study. Pooled 0.78-1.04)
optimal medical therapy; median time to angiography
605 received early CABG across the included studies was
and 642 received late found to be 3.43 h (1.47-5.40 h) in
CABG) the early strategy group and 41.3 h
(29.3-53.2 h) in the delayed
strategy group
Bernard et al. Retrospective Undefined 477 CABG, either as a 67 ± 12 < 4 30-day mortality Mortality was significantly higher for
[31]
(2023) cohort STEMI/NSTEMI STEMI: 162 first-line treatment patients who underwent CABG < 4
NSTEMI 315 or after angioplasty 5-10 Postoperative days compared to 5-10 days and ≥ 11
failure complications days (14% vs. 4.0% vs. 8.6%; P <
≥ 11 (LCOS, stroke, 0.01)
cardiogenic shock,
cardiac arrest, No difference between groups for
surgical re- postoperative complications
exploration)
SD: Standard deviation; ACS: acute coronary syndrome; AMI: acute myocardial infarction; CABG: coronary artery bypass grafting; LCOS: low-cardiac output syndrome; NSTE-ACS: non-ST-elevation acute coronary
syndrome; NSTEMI: non-ST-segment elevation myocardial infarction; OR: odds ratio; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction. Standard deviations have been
provided where available.
findings suggest that early revascularization may be detrimental to patients with non-cardiac comorbidities, conferring a higher surgical risk. A large cohort
study from Maganti et al. and a national retrospective study by Klempfner et al. similarly demonstrated the benefit of delaying surgical revascularization,
particularly in high-risk patients. This is consistent with the findings of a study by Lemaire et al. in which patients who underwent surgical revascularization
within 24 h were more likely to develop cardiac, renal, respiratory, and bleeding complications [35-37] .
Most of the literature on the optimal timing of surgical revascularization in patients with acute myocardial infarction has been derived from nonrandomized
data. Therefore, the burden of selection bias in these cohorts of patients is high. In other words, patients who required a surgical intervention earlier were more
likely to have a greater extent of ischemia and hemodynamic instability than those who could tolerate and survive a pre-operative waiting phase of a few days.
STEMI VERSUS NON-STEMI
The timing of surgery after AMI has also been evaluated relative to the type of myocardial infarction at presentation. The clinical course and treatment
strategies for STEMI and NSTEMI are often distinct, which may influence the optimal timing of surgical revascularization. In STEMI patients, there seems to