Page 122 - Read Online
P. 122
Zahrai et al. Vessel Plus 2023;7:32 https://dx.doi.org/10.20517/2574-1209.2023.100 Page 5 of 13
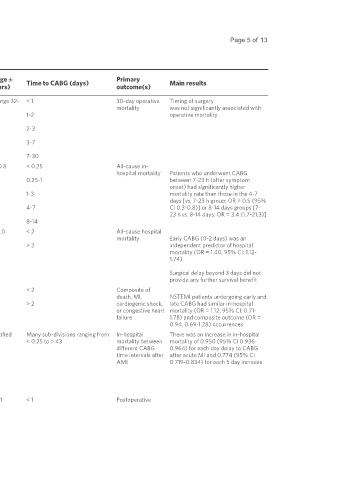
Table 3. Summary of the studies included
First Mean age ± Primary
author Study design MI type Number of patients Intervention(s) SD (years) Time to CABG (days) outcome(s) Main results
(year)
Sintek, et al. Retrospective STEMI, NSTEMI 2,175 (1,013 STEMI, # of Isolated CABG 63.4 (Range 32- < 1 30-day operative Timing of surgery
[41]
(1994) cohort NSTEMI not specified) 85) mortality was not significantly associated with
1-2 operative mortality
2-3
3-7
7-30
Thielmann Retrospective STEMI 138 Primary isolated 65.6 ± 10.8 < 0.25 All-cause in-
et al. cohort CABG hospital mortality Patients who underwent CABG
[39]
(2007) 0.25-1 between 7-23 h (after symptom
onset) had significantly higher
1-3 mortality rate than those in the 4-7
days [vs. 7-23 h group: OR = 0.5 (95%
4-7 CI 0.3-0.8)] or 8-14 days groups [7-
23 h vs. 8-14 days: OR = 3.4 (1.7-21.3)]
8-14
Weiss et al. Retrospective AMI type not 9,476 CABG of any type 67.6 ± 11.0 < 2 All-cause hospital
[7]
(2008) cohort specified mortality Early CABG (0-2 days) was an
> 2 independent predictor of hospital
mortality (OR = 1.40, 95% CI: 1.12-
1.74)
Surgical delay beyond 3 days did not
provide any further survival benefit
Parikh et al. Retrospective NSTEMI 2,647 CABG of any type 64.0 < 2 Composite of
[45]
(2010) cohort death, MI, NSTEMI patients undergoing early and
> 2 cardiogenic shock, late CABG had similar in-hospital
or congestive heart mortality (OR = 1.12, 95% CI: 0.71-
failure 1.78) and composite outcome (OR =
0.94, 0.69-1.28) occurrences
Chen et al. Meta-analysis 100,048 CABG of any type Not specified Many sub-divisions ranging from In-hospital There was an increase in in-hospital
[33]
(2014) of 12 studies STEMI (3 < 0.25 to > 43 mortality between mortality of 0.950 (95% CI 0.936-
studies different CABG 0.964) for each day delay to CABG
time intervals after after acute MI and 0.774 (95% CI
NSTEMI (1 AMI 0.719-0.834) for each 5 day increase
study)
STEMI/NSTEMI
(8 studies)
Lemaire et al. Retrospective STEMI 5,963 CABG of any type 63.1 ± 11.1 < 1 Postoperative
[37]
(2020)