Page 108 - Read Online
P. 108
Flattery et al. Vessel Plus 2024;8:26 https://dx.doi.org/10.20517/2574-1209.2023.130 Page 5 of 11
stable coronary artery disease with at least one CTO randomized incidence of overall MACE driven by decreased cardiac
after initial lesion crossing to IVUS optimization or angiography death or MI (HR 0.35, P = 0.035). No difference in TVR or
alone all-cause mortality
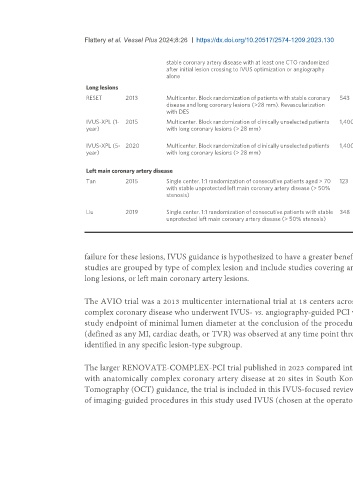
Long lesions
RESET 2013 Multicenter. Block randomization of patients with stable coronary 543 MACE (cardiovascular death, MI, ST, No significant difference in event rates between study
disease and long coronary lesions (>28 mm). Revascularization TVR) at one year groups
with DES
IVUS-XPL (1- 2015 Multicenter. Block randomization of clinically unselected patients 1,400 MACE (cardiac death, target lesion- Decreased incidence of MACE at one year (HR 0.48, P =
year) with long coronary lesions (> 28 mm) related MI, ischemia-driven TLR) at one 0.007), driven by decreased ischemia-driven TLR. No
year difference in definite or probable stent thrombosis
IVUS-XPL (5- 2020 Multicenter. Block randomization of clinically unselected patients 1,400 MACE (cardiac death, target lesion- Decreased incidence of MACE at five years (HR 0.50, p =
year) with long coronary lesions (> 28 mm) related MI, ischemia-driven TLR) at one 0.001), driven by decreased ischemia-driven TLR. No
year difference in definite or probable stent thrombosis
Left main coronary artery disease
Tan 2015 Single center. 1:1 randomization of consecutive patients aged > 70 123 Primary efficacy: two-year incidence of Decreased incidence of MACE at two years, driven by
with stable unprotected left main coronary artery disease (> 50% MACE (death, non-fatal MI, TLR) decreased rates of TLR (12.1% vs. 29.3%, P = 0.031). No
stenosis) Safety: ST significant difference in ST
Liu 2019 Single center. 1:1 randomization of consecutive patients with stable 348 Primary efficacy: one-year incidence of Decreased incidence of MACE at one year, driven by
unprotected left main coronary artery disease (> 50% stenosis) MACE (cardiac death, MI, TVR) decreased rate of cardiac death (13.2% vs. 21.9%, P =
Safety: ST 0.031). No significant difference in ST
failure for these lesions, IVUS guidance is hypothesized to have a greater benefit in these patients compared with its use in patients with simple lesions. These
studies are grouped by type of complex lesion and include studies covering any anatomically complex lesion (unselected), chronic total occlusions (CTOs),
long lesions, or left main coronary artery lesions.
The AVIO trial was a 2013 multicenter international trial at 18 centers across Europe, comparing procedural and clinical outcomes in 284 patients with
[11]
complex coronary disease who underwent IVUS- vs. angiography-guided PCI with DES . Though there was a statistically significant increase in the primary
study endpoint of minimal lumen diameter at the conclusion of the procedure in the IVUS group (2.70 vs. 2.51 mm, P = 0.0002), no reduction in MACE
(defined as any MI, cardiac death, or TVR) was observed at any time point through 24 months in the total study population, nor was there a signal for benefit
identified in any specific lesion-type subgroup.
The larger RENOVATE-COMPLEX-PCI trial published in 2023 compared intravascular imaging-guided PCI with angiography-guided PCI in 1,639 patients
with anatomically complex coronary artery disease at 20 sites in South Korea . Though the imaging group allowed either IVUS or Optical Coherence
[12]
Tomography (OCT) guidance, the trial is included in this IVUS-focused review, given its size, recent publication, and importance to the field. Moreover, 73%
of imaging-guided procedures in this study used IVUS (chosen at the operator’s discretion). Overall, at a median 2.1-year follow-up, there was a significant