Page 507 - Read Online
P. 507
Page 6 of 13 Mirastschijski et al. Plast Aesthet Res 2020;7:45 I http://dx.doi.org/10.20517/2347-9264.2020.44
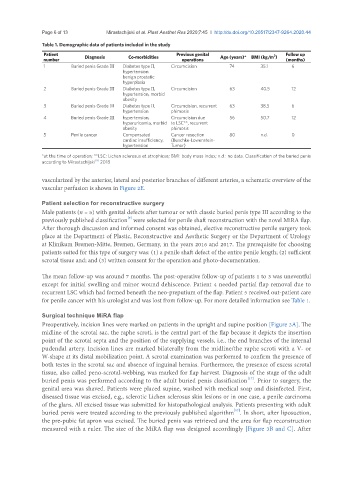
Table 1. Demographic data of patients included in the study
Patient Diagnosis Co-morbidities Previous genital Age (years)* BMI (kg/m ) Follow up
2
number operations (months)
1 Buried penis Grade III Diabetes type II, Circumcision 74 35.1 6
hypertension
benign prostatic
hyperplasia
2 Buried penis Grade III Diabetes type II, Circumcision 63 40.5 12
hypertension, morbid
obesity
3 Buried penis Grade III Diabetes type II, Circumcision, recurrent 63 38.5 6
hypertension phimosis
4 Buried penis Grade III hypertension, Circumcision due 56 50.7 12
hyperuricemia, morbid to LSC**, recurrent
obesity phimosis
5 Penile cancer Compensated Cancer resection 80 n.d. 0
cardiac insufficiency, (Buschke-Lowenstein-
hypertension Tumor)
*at the time of operation; **LSC: Lichen sclerosus et atrophicus; BMI: body mass index; n.d.: no data. Classification of the buried penis
[9]
according to Mirastschijski 2018
vascularized by the anterior, lateral and posterior branches of different arteries, a schematic overview of the
vascular perfusion is shown in Figure 2E.
Patient selection for reconstructive surgery
Male patients (n = 5) with genital defects after tumour or with classic buried penis type III according to the
[9]
previously published classification were selected for penile shaft reconstruction with the novel MiRA flap.
After thorough discussion and informed consent was obtained, elective reconstructive penile surgery took
place at the Department of Plastic, Reconstructive and Aesthetic Surgery or the Department of Urology
at Klinikum Bremen-Mitte, Bremen, Germany, in the years 2016 and 2017. The prerequisite for choosing
patients suited for this type of surgery was: (1) a penile shaft defect of the entire penile length; (2) sufficient
scrotal tissue and; and (3) written consent for the operation and photo-documentation.
The mean follow-up was around 7 months. The post-operative follow-up of patients 1 to 3 was uneventful
except for initial swelling and minor wound dehiscence. Patient 4 needed partial flap removal due to
recurrent LSC which had formed beneath the neo-preputium of the flap. Patient 5 received out-patient care
for penile cancer with his urologist and was lost from follow-up. For more detailed information see Table 1.
Surgical technique MiRA flap
Preoperatively, incision lines were marked on patients in the upright and supine position [Figure 3A]. The
midline of the scrotal sac, the raphe scroti, is the central part of the flap because it depicts the insertion
point of the scrotal septa and the position of the supplying vessels, i.e., the end branches of the internal
pudendal artery. Incision lines are marked bilaterally from the midline/the raphe scroti with a V- or
W-shape at its distal mobilization point. A scrotal examination was performed to confirm the presence of
both testes in the scrotal sac and absence of inguinal hernias. Furthermore, the presence of excess scrotal
tissue, also called peno-scrotal-webbing, was marked for flap harvest. Diagnosis of the stage of the adult
[17]
buried penis was performed according to the adult buried penis classification . Prior to surgery, the
genital area was shaved. Patients were placed supine, washed with medical soap and disinfected. First,
diseased tissue was excised, e.g., sclerotic Lichen sclerosus skin lesions or in one case, a penile carcinoma
of the glans. All excised tissue was submitted for histopathological analysis. Patients presenting with adult
[17]
buried penis were treated according to the previously published algorithm . In short, after liposuction,
the pre-pubic fat apron was excised. The buried penis was retrieved and the area for flap reconstruction
measured with a ruler. The size of the MiRA flap was designed accordingly [Figure 3B and C]. After