Page 95 - Read Online
P. 95
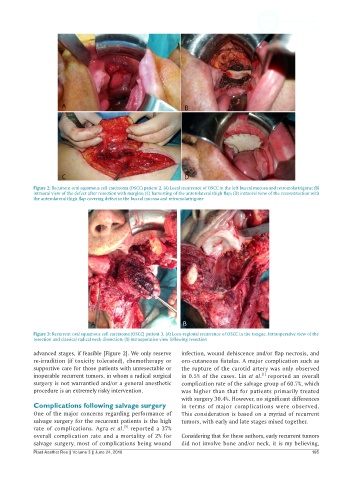
Figure 2: Recurrent oral squamous cell carcinoma (OSCC) patient 2. (A) Local recurrence of OSCC in the left buccal mucosa and retromolartrigone; (B)
intraoral view of the defect after resection with margins; (C) harvesting of the anterolateral thigh flap; (D) intraoral view of the reconstruction with
the anterolateral thigh flap covering defect in the buccal mucosa and retromolartrigone
Figure 3: Recurrent oral squamous cell carcinoma (OSCC) patient 3. (A) Loco-regional recurrence of OSCC in the tongue. Intraoperative view of the
resection and classical radical neck dissection; (B) intraoperative view following resection
advanced stages, if feasible [Figure 2]. We only reserve infection, wound dehiscence and/or flap necrosis, and
re-irradition (if toxicity tolerated), chemotherapy or oro-cutaneous fistulas. A major complication such as
supportive care for those patients with unresectable or the rupture of the carotid artery was only observed
[1]
inoperable recurrent tumors, in whom a radical surgical in 0.5% of the cases. Lin et al. reported an overall
surgery is not warrantied and/or a general anesthetic complication rate of the salvage group of 60.7%, which
procedure is an extremely risky intervention. was higher than that for patients primarily treated
with surgery 30.4%. However, no significant differences
Complications following salvage surgery in terms of major complications were observed.
One of the major concerns regarding performance of This consideration is based on a myriad of recurrent
salvage surgery for the recurrent patients is the high tumors, with early and late stages mixed together.
[5]
rate of complications. Agra et al. reported a 37%
overall complication rate and a mortality of 2% for Considering that for these authors, early recurrent tumors
salvage surgery, most of complications being wound did not involve bone and/or neck, it is my believing,
Plast Aesthet Res || Volume 3 || June 24, 2016 195