Page 52 - Read Online
P. 52
Page 10 of 17 Qiu et al. Plast Aesthet Res 2022;9:19 https://dx.doi.org/10.20517/2347-9264.2021.126
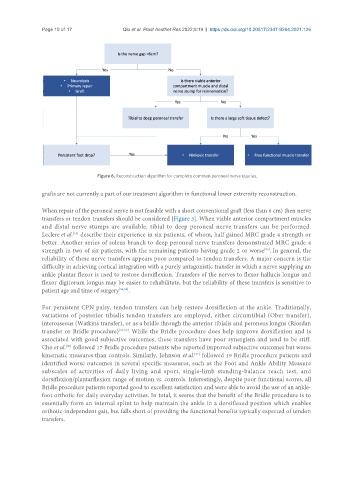
Figure 6. Reconstruction algorithm for complete common peroneal nerve injuries.
grafts are not currently a part of our treatment algorithm in functional lower extremity reconstruction.
When repair of the peroneal nerve is not feasible with a short conventional graft (less than 6 cm) then nerve
transfers or tendon transfers should be considered [Figure 3]. When viable anterior compartment muscles
and distal nerve stumps are available, tibial to deep peroneal nerve transfers can be performed.
Leclere et al. describe their experience in six patients, of whom, half gained MRC grade 4 strength or
[51]
better. Another series of soleus branch to deep peroneal nerve transfers demonstrated MRC grade 4
strength in two of six patients, with the remaining patients having grade 2 or worse . In general, the
[52]
reliability of these nerve transfers appears poor compared to tendon transfers. A major concern is the
difficulty in achieving cortical integration with a purely antagonistic transfer in which a nerve supplying an
ankle plantar flexor is used to restore dorsiflexion. Transfers of the nerves to flexor hallucis longus and
flexor digitorum longus may be easier to rehabilitate, but the reliability of these transfers is sensitive to
patient age and time of surgery [53,54] .
For persistent CPN palsy, tendon transfers can help restore dorsiflexion at the ankle. Traditionally,
variations of posterior tibialis tendon transfers are employed, either circumtibial (Ober transfer),
interosseous (Watkins transfer), or as a bridle through the anterior tibialis and peroneus longus (Riordan
transfer or Bridle procedure) [55-59] . While the Bridle procedure does help improve dorsiflexion and is
associated with good subjective outcomes, these transfers have poor synergism and tend to be stiff.
[60]
Cho et al. followed 17 Bridle procedure patients who reported improved subjective outcomes but worse
kinematic measures than controls. Similarly, Johnson et al. followed 19 Bridle procedure patients and
[61]
identified worse outcomes in several specific measures, such as the Foot and Ankle Ability Measure
subscales of activities of daily living and sport, single-limb standing-balance reach test, and
dorsiflexion/plantarflexion range of motion vs. controls. Interestingly, despite poor functional scores, all
Bridle procedure patients reported good to excellent satisfaction and were able to avoid the use of an ankle-
foot orthotic for daily everyday activities. In total, it seems that the benefit of the Bridle procedure is to
essentially form an internal splint to help maintain the ankle in a dorsiflexed position which enables
orthotic-independent gait, but falls short of providing the functional benefits typically expected of tendon
transfers.