Page 34 - Read Online
P. 34
Page 10 of 17 Toyoda et al. Plast Aesthet Res 2022;9:17 https://dx.doi.org/10.20517/2347-9264.2021.118
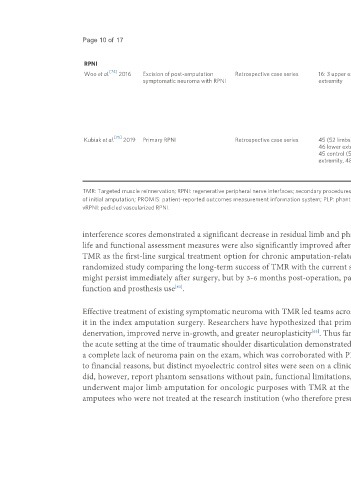
RPNI
[74]
Woo et al. 2016 Excision of post-amputation Retrospective case series 16: 3 upper extremity, 14 lower • Mean follow up 7.5 months • 81% able to wear prosthesis after
symptomatic neuroma with RPNI extremity • Postoperative phone interviews with RPNI (vs. 56% preoperatively)
patient-reported pains cores adapted from • Average pain score reduction 71%
PROMIS • 56% reduced pain medication use
• 100% response rate (none increased)
• Aggregate pain interference score
2.15 (vs. 4.6 preoperatively)
• 75% satisfied
• 94% would have surgery again
[75]
Kubiak et al. 2019 Primary RPNI Retrospective case series 45 (52 limbs): 6 upper extremity, • Mean follow up 357 days • 13.3% of control patients developed
46 lower extremity • Pain outcomes binary symptomatic neuromas
45 control (52 limbs): 4 upper • 0% of primary RPNI patients
extremity, 48 lower extremity developed symptomatic neuromas
• 51% of primary RPNI patients
developed PLP
TMR: Targeted muscle reinnervation; RPNI: regenerative peripheral nerve interfaces; secondary procedures: treatment of postamputation symptomatic neuromas; primary procedures: prophylactic treatment at time
of initial amputation; PROMIS: patient-reported outcomes measurement information system; PLP: phantom limb pain; NRS: numerical rating scale; OPUS: orthotics prosthetics users survey; QOL: quality of life;
vRPNI: pedicled vascularized RPNI.
interference scores demonstrated a significant decrease in residual limb and phantom limb pains at one-year follow-up compared to preoperatively. Quality of
life and functional assessment measures were also significantly improved after TMR for both upper and lower extremity amputees. The authors recommend
[62]
TMR as the first-line surgical treatment option for chronic amputation-related pain . Bowen et al. are performing an ongoing prospective multicenter,
[63]
randomized study comparing the long-term success of TMR with the current standard of care. Preliminary results demonstrated that neuroma pain and PLP
might persist immediately after surgery, but by 3-6 months post-operation, patients can expect reduced pain, less inhibition from PLP, and improvement in
function and prosthesis use .
[63]
Effective treatment of existing symptomatic neuroma with TMR led teams across the country to assess its effect on neuroma pain prophylaxis by incorporating
it in the index amputation surgery. Researchers have hypothesized that primary TMR has the advantages of decreased muscle atrophy due to less muscle
denervation, improved nerve in-growth, and greater neuroplasticity . Thus far, primary TMR has demonstrated promising results. The first report of TMR in
[63]
the acute setting at the time of traumatic shoulder disarticulation demonstrated multiple successful nerve transfers for myoelectric prosthesis control as well as
a complete lack of neuroma pain on the exam, which was corroborated with PROMIS at 8 months post-operation . The patient did not use a prosthesis due
[64]
[64]
to financial reasons, but distinct myoelectric control sites were seen on a clinical exam when she was able to trigger contraction under cortical control . She
did, however, report phantom sensations without pain, functional limitations, and mood depression . In another study by Alexander et al. , patients who
[65]
[64]
underwent major limb amputation for oncologic purposes with TMR at the time of amputation were compared to a cross-sectional sample of oncologic
amputees who were not treated at the research institution (who therefore presumably had amputations without TMR). At one year follow-up, those who had