Page 33 - Read Online
P. 33
Toyoda et al. Plast Aesthet Res 2022;9:17 https://dx.doi.org/10.20517/2347-9264.2021.118 Page 9 of 17
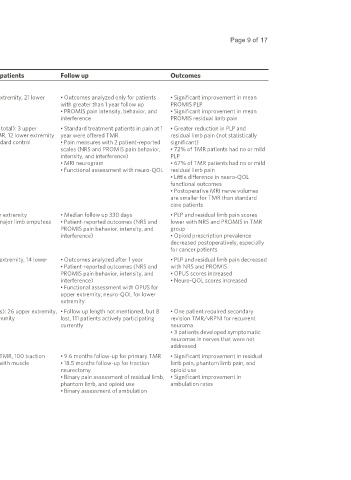
Table 1. Summary of clinical outcomes data in TMR and RPNI of the lower extremity
Authors, year Technique Study design Number of patients Follow up Outcomes
TMR
[65]
Alexander et al. Primary TMR for upper and lower Retrospective case series 27: 6 upper extremity, 21 lower • Outcomes analyzed only for patients • Significant improvement in mean
2019 extremity oncologic amputation extremity with greater than 1 year follow up PROMIS PLP
• PROMIS pain intensity, behavior, and • Significant improvement in mean
interference PROMIS residual limb pain
[27]
Dumanian et al. Excision of post-amputation Prospective, single-blinded, 28 (30 limbs total): 3 upper • Standard treatment patients in pain at 1 • Greater reduction in PLP and
2019 symptomatic neuroma with TMR randomized clinical trial extremity TMR, 12 lower extremity year were offered TMR residual limb pain (not statistically
TMR, 15 standard control • Pain measures with 2 patient-reported significant)
scales (NRS and PROMIS pain behavior, • 72% of TMR patients had no or mild
intensity, and interference) PLP
• MRI neurogram • 67% of TMR patients had no or mild
• Functional assessment with neuro-QOL residual limb pain
• Little difference in neuro-QOL
functional outcomes
• Postoperative MRI nerve volumes
are smaller for TMR than standard
care patients
[66]
Valerio et al. 2019 Primary TMR or secondary TMR Retrospective multi- 51: 71% lower extremity • Median follow up 330 days • PLP and residual limb pain scores
within 14 days of initial amputation institutional cohort study 438 control major limb amputees • Patient-reported outcomes (NRS and lower with NRS and PROMIS in TMR
PROMIS pain behavior, intensity, and group
interference) • Opioid prescription prevalence
decreased postoperatively, especially
for cancer patients
[62]
Mioton et al. 2020 Secondary TMR Prospective cohort study 33: 19 upper extremity, 14 lower • Outcomes analyzed after 1 year • PLP and residual limb pain decreased
extremity • Patient-reported outcomes (NRS and with NRS and PROMIS
PROMIS pain behavior, intensity, and • OPUS scores increased
interference) • Neuro-QOL scores increased
• Functional assessment with OPUS for
upper extremity, neuro-QOL for lower
extremity
[76]
Valerio et al. 2020 Primary (76%) and secondary Retrospective multi- 119 (123 limbs): 26 upper extremity, • Follow up length not mentioned, but 8 • One patient required secondary
(24%) TMR/vRPNI institutional cohort study 93 lower extremity lost, 111 patients actively participating revision TMR/vRPNI for recurrent
currently neuroma
• 3 patients developed symptomatic
neuromas in nerves that were not
addressed
[67]
Chang et al. 2021 Primary TMR vs. traction Retrospective single-surgeon, 100 primary TMR, 100 traction • 9.6 months follow-up for primary TMR • Significant improvement in residual
neurectomy with muscle single-institution comparative neurectomy with muscle • 18.5 months follow-up for traction limb pain, phantom limb pain, and
implantation in vasculopathic BKA cohort study implantation neurectomy opioid use
• Binary pain assessment of residual limb, • Significant improvement in
phantom limb, and opioid use ambulation rates
• Binary assessment of ambulation