Page 22 - Read Online
P. 22
Hicks et al. Plast Aesthet Res 2022;9:2 https://dx.doi.org/10.20517/2347-9264.2021.65 Page 3 of 11
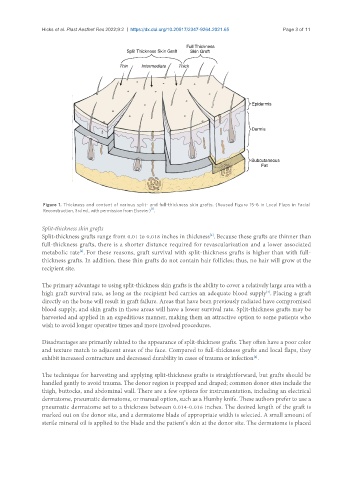
Figure 1. Thickness and content of various split- and full-thickness skin grafts. (Reused Figure 15-6 in Local Flaps in Facial
[1]
Reconstruction, 3rd ed., with permission from Elsevier) .
Split-thickness skin grafts
Split-thickness grafts range from 0.01 to 0.018 inches in thickness . Because these grafts are thinner than
[4]
full-thickness grafts, there is a shorter distance required for revascularization and a lower associated
metabolic rate . For these reasons, graft survival with split-thickness grafts is higher than with full-
[4]
thickness grafts. In addition, these thin grafts do not contain hair follicles; thus, no hair will grow at the
recipient site.
The primary advantage to using split-thickness skin grafts is the ability to cover a relatively large area with a
[4]
high graft survival rate, as long as the recipient bed carries an adequate blood supply . Placing a graft
directly on the bone will result in graft failure. Areas that have been previously radiated have compromised
blood supply, and skin grafts in these areas will have a lower survival rate. Split-thickness grafts may be
harvested and applied in an expeditious manner, making them an attractive option to some patients who
wish to avoid longer operative times and more involved procedures.
Disadvantages are primarily related to the appearance of split-thickness grafts. They often have a poor color
and texture match to adjacent areas of the face. Compared to full-thickness grafts and local flaps, they
exhibit increased contracture and decreased durability in cases of trauma or infection .
[4]
The technique for harvesting and applying split-thickness grafts is straightforward, but grafts should be
handled gently to avoid trauma. The donor region is prepped and draped; common donor sites include the
thigh, buttocks, and abdominal wall. There are a few options for instrumentation, including an electrical
dermatome, pneumatic dermatome, or manual option, such as a Humby knife. These authors prefer to use a
pneumatic dermatome set to a thickness between 0.014-0.016 inches. The desired length of the graft is
marked out on the donor site, and a dermatome blade of appropriate width is selected. A small amount of
sterile mineral oil is applied to the blade and the patient’s skin at the donor site. The dermatome is placed