Page 88 - Read Online
P. 88
Page 266 Yoshimura et al. Neuroimmunol Neuroinflammation 2020;7:264-76 I http://dx.doi.org/10.20517/2347-8659.2020.22
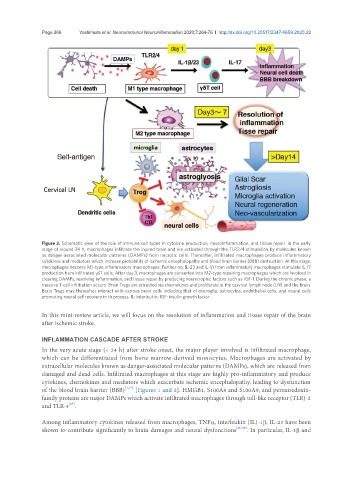
Figure 2. Schematic view of the role of immune cell types in cytokine production, neuroinflammation, and tissue repair. In the early
stage of around 24 h, macrophages infiltrate the injured brain and are activated through the TLR2/4 stimulation by molecules known
as danger-associated molecular patterns (DAMPs) from necrotic cells. Thereafter, infiltrated macrophages produce inflammatory
cytokines and mediators which increase probability of ischemic encephalopathy and blood brain barrier (BBB) destruction. At this stage,
macrophages become M1-type inflammatory macrophages. Further on, IL-23 and IL-1β from inflammatory macrophages stimulate IL-17
production from infiltrated γδT cells. After day 3, macrophages are converted into M2-type repairing macrophages which are involved in
clearing DAMPs, resolving inflammation, and tissue repair by producing neurotrophic factors such as IGF-1. During the chronic phase, a
massive T-cell infiltration occurs. Brain Tregs are attracted via chemokines and proliferate in the cervical lymph node (LN) and the brain.
Brain Tregs may thereafter interact with various brain cells including that of microglia, astrocytes, endothelial cells, and neural cells
promoting neural cell recovery in th process. IL: interleukin; IGF: insulin growth factor
In this mini-review article, we will focus on the resolution of inflammation and tissue repair of the brain
after ischemic stroke.
INFLAMMATION CASCADE AFTER STROKE
In the very acute stage (< 24 h) after stroke onset, the major player involved is infiltrated macrophage,
which can be differentiated from bone marrow-derived monocytes. Macrophages are activated by
extracellular molecules known as danger-associated molecular patterns (DAMPs), which are released from
damaged and dead cells. Infiltrated macrophages at this stage are highly pro-inflammatory and produce
cytokines, chemokines and mediators which exacerbate ischemic encephalopathy, leading to dysfunction
of the blood brain barrier (BBB) [4,14] [Figures 1 and 2]. HMGB1, S100A8 and S100A9, and peroxiredoxin-
family proteins are major DAMPs which activate infiltrated macrophages through toll-like receptor (TLR)-2
[15]
and TLR-4 .
Among inflammatory cytokines released from macrophages, TNFα, interleukin (IL)-1β, IL-23 have been
shown to contribute significantly to brain damages and neural dysfunctions [16-19] . In particular, IL-1β and