Page 111 - Read Online
P. 111
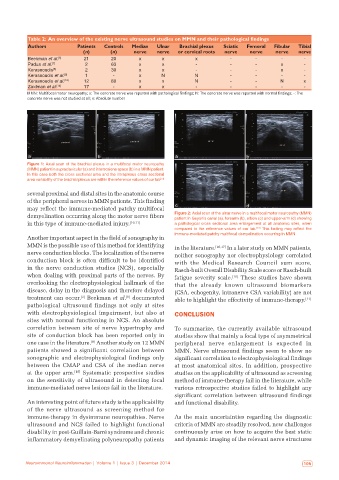
Table 2: An overview of the existing nerve ultrasound studies on MMN and their pathological findings
Authors Patients Controls Median Ulnar Brachial plexus Sciatic Femoral Fibular Tibial
(n) (n) nerve nerve or cervical roots nerve nerve nerve nerve
Beekman et al. [6] 21 20 x x x ‑ ‑ ‑ ‑
Padua et al. [7] 2 63 x x ‑ ‑ ‑ x ‑
Kerasnoudis [8] 2 30 x x ‑ ‑ ‑ x ‑
Kerasnoudis et al. [9] 1 ‑ x N N ‑ ‑ ‑ ‑
Kerasnoudis et al. [10] 12 80 x x N ‑ ‑ N x
Zaidman et al. [14] 17 ‑ x x ‑ ‑ ‑ ‑ ‑
MMN: Multifocal motor neuropathy; x: The concrete nerve was reported with pathological findings; N: The concrete nerve was reported with normal findings; -: The
concrete nerve was not studied at all; n: Absolute number
a b a b
Figure 1: Axial scan of the brachial plexus in a multifocal motor neuropathy
(MMN) patient in supraclavicular (a) and interscalene space (b) in a MMN patient.
In this case both the cross sectional area and the intraplexus cross sectional
area variability of the brachial plexus are within the reference values of our lab
[13]
several proximal and distal sites in the anatomic course
of the peripheral nerves in MMN patients. This finding
may reflect the immune-mediated patchy multifocal c d
demyelination occurring along the motor nerve fibers Figure 2: Axial scan of the ulnar nerve in a multifocal motor neuropathy (MMN)
patient in Guyon’s canal (a), forearm (b), elbow (c) and upper‑arm (d) showing
in this type of immune-mediated injury. [10,11] a pathological cross sectional area enlargement at all anatomic sites, when
[13]
compared to the reference values of our lab. This finding may reflect the
immune‑mediated patchy multifocal demyelination occurring in MMN
Another important aspect in the field of sonography in
MMN is the possible use of this method for identifying in the literature. [16,17] In a later study on MMN patients,
nerve conduction blocks. The localization of the nerve neither sonography nor electrophysiology correlated
conduction block is often difficult to be identified with the Medical Research Council sum score,
in the nerve conduction studies (NCS), especially Rasch-built Overall Disability Scale score or Rasch-built
when dealing with proximal parts of the nerves. By fatigue severity scale. [10] These studies have shown
overlooking the electrophysiological hallmark of the that the already known ultrasound biomarkers
disease, delay in the diagnosis and therefore delayed (CSA, echogenity, intranerve CSA variability) are not
treatment can occur. Beekman et al. documented able to highlight the effectivity of immune-therapy. [11]
[6]
[2]
pathological ultrasound findings not only at sites
with electrophysiological impairment, but also at CONCLUSION
sites with normal functioning in NCS. An absolute
correlation between site of nerve hypertrophy and To summarize, the currently available ultrasound
site of conduction block has been reported only in studies show that mainly a focal type of asymmetrical
[8]
one case in the literature. Another study on 12 MMN peripheral nerve enlargement is expected in
patients showed a significant correlation between MMN. Nerve ultrasound findings seem to show no
sonographic and electrophysiological findings only significant correlation to electrophysiological findings
between the CMAP and CSA of the median nerve at most anatomical sites. In addition, prospective
at the upper arm. [10] Systematic prospective studies studies on the applicability of ultrasound as screening
on the sensitivity of ultrasound in detecting focal method of immune-therapy fail in the literature, while
immune-mediated nerve lesions fail in the literature. various retrospective studies failed to highlight any
significant correlation between ultrasound findings
An interesting point of future study is the applicability and functional disability.
of the nerve ultrasound as screening method for
immune-therapy in dysimmune neuropathies. Nerve As the main uncertainties regarding the diagnostic
ultrasound and NCS failed to highlight functional criteria of MMN are steadily resolved, new challenges
disability in post-Guillain-Barré syndrome and chronic continuously arise on how to acquire the best static
inflammatory demyelinating polyneuropathy patients and dynamic imaging of the relevant nerve structures
Neuroimmunol Neuroinflammation | Volume 1 | Issue 3 | December 2014 105