Page 196 - Read Online
P. 196
Kolokotronis et al. Mini-invasive Surg 2021;5:19 https://dx.doi.org/10.20517/2574-1225.2021.07 Page 9 of 11
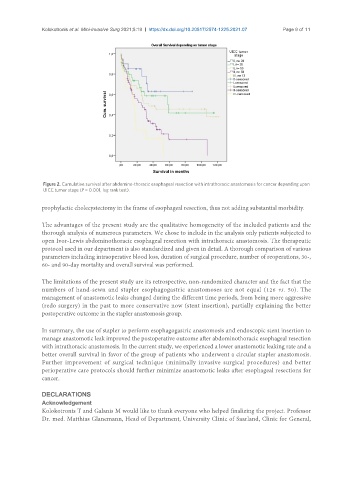
Figure 2. Cumulative survival after abdomino-thoracic esophageal resection with intrathoracic anastomosis for cancer depending upon
UICC tumor stage (P = 0.001, log rank test).
prophylactic cholecystectomy in the frame of esophageal resection, thus not adding substantial morbidity.
The advantages of the present study are the qualitative homogeneity of the included patients and the
thorough analysis of numerous parameters. We chose to include in the analysis only patients subjected to
open Ivor-Lewis abdominothoracic esophageal resection with intrathoracic anastomosis. The therapeutic
protocol used in our department is also standardized and given in detail. A thorough comparison of various
parameters including intraoperative blood loss, duration of surgical procedure, number of reoperations, 30-,
60- and 90-day mortality and overall survival was performed.
The limitations of the present study are its retrospective, non-randomized character and the fact that the
numbers of hand-sewn and stapler esophagogastric anastomoses are not equal (126 vs. 50). The
management of anastomotic leaks changed during the different time periods, from being more aggressive
(redo surgery) in the past to more conservative now (stent insertion), partially explaining the better
postoperative outcome in the stapler anastomosis group.
In summary, the use of stapler to perform esophagogastric anastomosis and endoscopic stent insertion to
manage anastomotic leak improved the postoperative outcome after abdominothoracic esophageal resection
with intrathoracic anastomosis. In the current study, we experienced a lower anastomotic leaking rate and a
better overall survival in favor of the group of patients who underwent a circular stapler anastomosis.
Further improvement of surgical technique (minimally invasive surgical procedures) and better
perioperative care protocols should further minimize anastomotic leaks after esophageal resections for
cancer.
DECLARATIONS
Acknowledgement
Kolokotronis T and Galanis M would like to thank everyone who helped finalizing the project. Professor
Dr. med. Matthias Glanemann, Head of Department, University Clinic of Saarland, Clinic for General,