Page 194 - Read Online
P. 194
Kolokotronis et al. Mini-invasive Surg 2021;5:19 https://dx.doi.org/10.20517/2574-1225.2021.07 Page 7 of 11
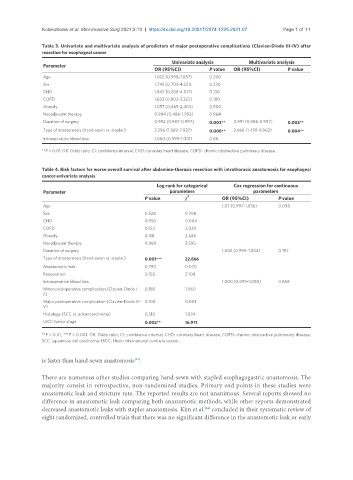
Table 3. Univariate and multivariate analysis of predictors of major postoperative complications (Clavien-Dindo III-IV) after
resection for esophageal cancer
Univariate analysis Multivariate analysis
Parameter
OR (95%CI) P value OR (95%CI) P value
Age 1.022 (0.998-1.057) 0.200
Sex 1.745 (0.703-4.331) 0.230
CHD 1.847 (0.838-4.071) 0.130
COPD 1.633 (0.802-3.327) 0.180
Obesity 1.057 (0.465-2.403) 0.900
Neoadjuvant therapy 0.984 (0.486-1.993) 0.964
Duration of surgery 0.992 (0.987-0.997) 0.003** 0.991 (0.986-0.997) 0.002**
Type of anastomosis (hand-sewn vs. stapler) 3.296 (1.369-7.937) 0.008** 3.666 (1.499-8.963) 0.004**
Intraoperative blood loss 1.000 (0.999-1.001) 0.68
**P < 0.01. OR: Odds ratio; CI: confidence interval; CHD: coronary heart disease; COPD: chronic obstructive pulmonary disease.
Table 4. Risk factors for worse overall survival after abdomino-thoracic resection with intrathoracic anastomosis for esophageal
cancer-univariate analysis
Log rank for categorical Cox regression for continuous
Parameter parameters parameters
P value χ 2 OR (95%CI) P value
Age 1.07 (0.997-1.036) 0.098
Sex 0.528 0.398
CHD 0.950 0.004
COPD 0.153 2.039
Obesity 0.118 2.446
Neoadjuvant therapy 0.060 3.595
Duration of surgery 1.002 (0.999-1.004) 0.197
Type of anastomosis (hand-sewn vs. stapler) 0.001*** 22.866
Anastomotic leak 0.790 0.070
Reoperation 0.150 2.108
Intraoperative blood loss 1.000 (0.999-1.000) 0.658
Minor postoperative complication (Clavien-Dindo I- 0.810 1.060
II)
Major postoperative complication (Clavien-Dindo III- 0.100 0.001
V)
Histology (SCC vs. adenocarcinoma) 0.310 1.034
UICC tumor stage 0.002** 16.971
**P < 0.01, ***P < 0.001. OR: Odds ratio; CI: confidence interval; CHD: coronary heart disease; COPD: chronic obstructive pulmonary disease;
SCC: squamous cell carcinoma; UICC: Union international contre le cancer.
is faster than hand-sewn anastomosis .
[24]
There are numerous other studies comparing hand-sewn with stapled esophagogastric anastomosis. The
majority consist in retrospective, non-randomized studies. Primary end points in these studies were
anastomotic leak and stricture rate. The reported results are not unanimous. Several reports showed no
difference in anastomotic leak comparing both anastomotic methods, while other reports demonstrated
decreased anastomotic leaks with stapler anastomosis. Kim et al. concluded in their systematic review of
[24]
eight randomized, controlled trials that there was no significant difference in the anastomotic leak or early