Page 73 - Read Online
P. 73
Page 6 of 11 Shimada et al. Mini-invasive Surg 2019;3:7 I http://dx.doi.org/10.20517/2574-1225.2018.78
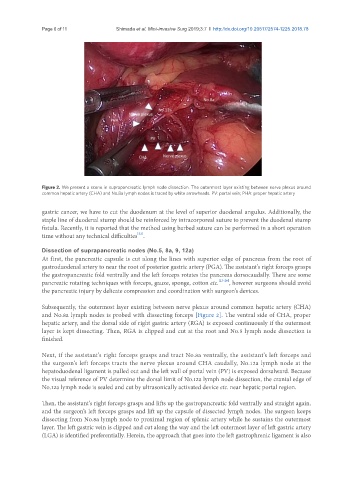
Figure 2. We present a scene in suprapancreatic lymph node dissection. The outermost layer existing between nerve plexus around
common hepatic artery (CHA) and No.8a lymph nodes is traced by white arrowheads. PV: portal vein; PHA: proper hepatic artery
gastric cancer, we have to cut the duodenum at the level of superior duodenal angulus. Additionally, the
staple line of duodenal stump should be reinforced by intracorporeal suture to prevent the duodenal stump
fistula. Recently, it is reported that the method using barbed suture can be performed in a short operation
[22]
time without any technical difficulties .
Dissection of suprapancreatic nodes (No.5, 8a, 9, 12a)
At first, the pancreatic capsule is cut along the lines with superior edge of pancreas from the root of
gastroduodenal artery to near the root of posterior gastric artery (PGA). The assistant’s right forceps grasps
the gastropancreatic fold ventrally and the left forceps rotates the pancreas dorsocaudally. There are some
pancreatic rotating techniques with forceps, gauze, sponge, cotton etc. [23-26] , however surgeons should avoid
the pancreatic injury by delicate compression and coordination with surgeon’s devices.
Subsequently, the outermost layer existing between nerve plexus around common hepatic artery (CHA)
and No.8a lymph nodes is probed with dissecting forceps [Figure 2]. The ventral side of CHA, proper
hepatic artery, and the dorsal side of right gastric artery (RGA) is exposed continuously if the outermost
layer is kept dissecting. Then, RGA is clipped and cut at the root and No.5 lymph node dissection is
finished.
Next, if the assistant’s right forceps grasps and tract No.8a ventrally, the assistant’s left forceps and
the surgeon’s left forceps tracts the nerve plexus around CHA caudally, No.12a lymph node at the
hepatoduodenal ligament is pulled out and the left wall of portal vein (PV) is exposed dorsalward. Because
the visual reference of PV determine the dorsal limit of No.12a lymph node dissection, the cranial edge of
No.12a lymph node is sealed and cut by ultrasonically activated device etc. near hepatic portal region.
Then, the assistant’s right forceps grasps and lifts up the gastropancreatic fold ventrally and straight again,
and the surgeon’s left forceps grasps and lift up the capsule of dissected lymph nodes. The surgeon keeps
dissecting from No.8a lymph node to proximal region of splenic artery while he sustains the outermost
layer. The left gastric vein is clipped and cut along the way and the left outermost layer of left gastric artery
(LGA) is identified preferentially. Herein, the approach that goes into the left gastrophrenic ligament is also