Page 37 - Read Online
P. 37
Wagaskar et al. Mini-invasive Surg 2022;6:14 https://dx.doi.org/10.20517/2574-1225.2021.106 Page 5 of 8
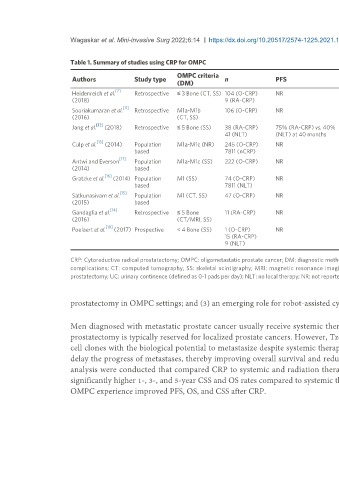
Table 1. Summary of studies using CRP for OMPC
OMPC criteria Functional
Authors Study type n PFS CSS OS SRC (details)
(DM) outcome
[7]
Heidenreich et al. Retrospective ≤ 3 Bone (CT, SS) 104 (O-CRP) NR 89% at 3 years; 81% at 80% at 5 years 68% UC at 12 9% (5% - RL for bleeding; 4%-
(2018) 9 (RA-CRP) 5 years months LD)
[11]
Sooriakumaran et al. Retrospective M1a-M1b 106 (O-CRP) NR NR 89% at 23 months 64% UC at 3 19% (14%-BT; 5%-LD)
(2016) (CT, SS) months
[12]
Jang et al. (2018) Retrospective ≤ 5 Bone (SS) 38 (RA-CRP) 75% (RA-CRP) vs. 40% NR NR NR 13% (8%-BT; 5%-RL for rectal
41 (NLT) (NLT) at 40 months injury; bleeding)
[13]
Culp et al. (2014) Population M1a-M1c (NR) 245 (O-CRP) NR 76% (RP) vs. 61% 67% (RP) vs. 53% NR NR
based 7811 (nCRP) (nCRP) at 5 years (nCRP) at 5 years
[17]
Antwi and Everson Population M1a-M1c (SS) 222 (O-CRP) NR 85% 82% NR NR
(2014) based
[16]
Gratzke et al. (2014) Population M1 (SS) 74 (O-CRP) NR NR 55% (RP) vs. 21% NR NR
based 7811 (NLT) (NLT) at 5 years
[15]
Satkunasivam et al. Population M1 (CT, SS) 47 (O-CRP) NR 79% at 3 years 73% at 3 years NR NR
(2015) based
[14]
Gandaglia et al. Retrospective ≤ 5 Bone 11 (RA-CRP) NR 82% at 7 years NR NR 82% (73%-BT, 9%-RL for
(2016) (CT/MRI, SS) anastomotic leakage)
[18]
Poelaert et al. (2017) Prospective < 4 Bone (SS) 1 (O-CRP) NR 100% (RP) vs. 61% 100% (RP) vs. 51% 49% UC at 3 0%
15 (RA-CRP) (NLT) at 2 years (NLT) at 2 years months
9 (NLT)
CRP: Cytoreductive radical prostatectomy; OMPC: oligometastatic prostate cancer; DM: diagnostic method; PFS: progression-free survival; CSS: cancer-specific survival; OS: overall survival; SRC: surgery-related
complications; CT: computed tomography; SS: skeletal scintigraphy; MRI: magnetic resonance imaging; O-CRP: open cytoreductive radical prostatectomy; RA-CRP: robot-assisted cytoreductive radical
prostatectomy; UC: urinary continence (defined as 0-1 pads per day); NLT: no local therapy; NR: not reported; RL: repeat laparotomy; LD: lymphocele drainage; BT: blood transfusion.
prostatectomy in OMPC settings; and (3) an emerging role for robot-assisted cytoreductive prostatectomy in selected men with OMPC.
Men diagnosed with metastatic prostate cancer usually receive systemic therapy, such as androgen deprivation therapy and chemotherapy, while radical
prostatectomy is typically reserved for localized prostate cancers. However, Tzelepi et al. demonstrated the intra-prostatic survival of lethal prostate cancer
[21]
cell clones with the biological potential to metastasize despite systemic therapy. A growing body of evidence suggests that control of a primary tumor may
delay the progress of metastases, thereby improving overall survival and reducing prostate cancer-specific mortality. Recently systematic review and meta-
analysis were conducted that compared CRP to systemic and radiation therapy in the treatment of OMPC. This systematic review showed that CRP had
[22]
significantly higher 1-, 3-, and 5-year CSS and OS rates compared to systemic therapy . This review of the current literature also demonstrated that men with
OMPC experience improved PFS, OS, and CSS after CRP.