Page 46 - Read Online
P. 46
Chandrasekar et al. Mini-invasive Surg 2021;5:33 https://dx.doi.org/10.20517/2574-1225.2021.12 Page 9 of 16
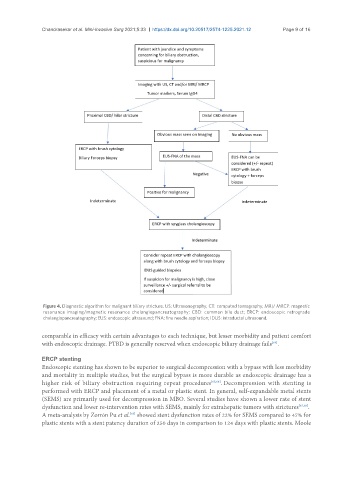
Figure 4. Diagnostic algorithm for malignant biliary stricture. US: Ultrasonography; CT: computed tomography; MRI/ MRCP: magnetic
resonance imaging/magnetic resonance cholangiopancreatography; CBD: common bile duct; ERCP: endoscopic retrograde
cholangiopancreatography; EUS: endoscopic ultrasound; FNA: fine needle aspiration; IDUS: intraductal ultrasound.
comparable in efficacy with certain advantages to each technique, but lesser morbidity and patient comfort
with endoscopic drainage. PTBD is generally reserved when endoscopic biliary drainage fails .
[64]
ERCP stenting
Endoscopic stenting has shown to be superior to surgical decompression with a bypass with less morbidity
and mortality in multiple studies, but the surgical bypass is more durable as endoscopic drainage has a
higher risk of biliary obstruction requiring repeat procedures [65,66] . Decompression with stenting is
performed with ERCP and placement of a metal or plastic stent. In general, self-expandable metal stents
(SEMS) are primarily used for decompression in MBO. Several studies have shown a lower rate of stent
dysfunction and lower re-intervention rates with SEMS, mainly for extrahepatic tumors with strictures [67,68] .
[69]
A meta-analysis by Zorrón Pu et al. showed stent dysfunction rates of 22% for SEMS compared to 47% for
plastic stents with a stent patency duration of 250 days in comparison to 124 days with plastic stents. Moole