Page 30 - Read Online
P. 30
Shirakawa et al. Mini-invasive Surg 2020;4:33 I http://dx.doi.org/10.20517/2574-1225.2020.30 Page 7 of 9
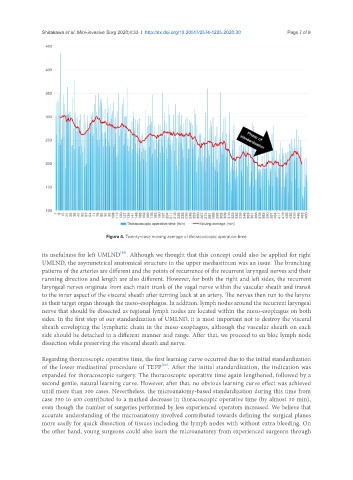
Figure 4. Twenty-case moving average of thoracoscopic operative time
[19]
its usefulness for left UMLND . Although we thought that this concept could also be applied for right
UMLND, the asymmetrical anatomical structure in the upper mediastinum was an issue. The branching
patterns of the arteries are different and the points of recurrence of the recurrent laryngeal nerves and their
running direction and length are also different. However, for both the right and left sides, the recurrent
laryngeal nerves originate from each main trunk of the vagal nerve within the vascular sheath and transit
to the inner aspect of the visceral sheath after turning back at an artery. The nerves then run to the larynx
as their target organ through the meso-esophagus. In addition, lymph nodes around the recurrent laryngeal
nerve that should be dissected as regional lymph nodes are located within the meso-esophagus on both
sides. In the first step of our standardization of UMLND, it is most important not to destroy the visceral
sheath enveloping the lymphatic chain in the meso-esophagus, although the vascular sheath on each
side should be detached in a different manner and range. After that, we proceed to en bloc lymph node
dissection while preserving the visceral sheath and nerve.
Regarding thoracoscopic operative time, the first learning curve occurred due to the initial standardization
[20]
of the lower mediastinal procedure of TEPP . After the initial standardization, the indication was
expanded for thoracoscopic surgery. The thoracoscopic operative time again lengthened, followed by a
second gentle, natural learning curve. However, after that, no obvious learning curve effect was achieved
until more than 300 cases. Nevertheless, the microanatomy-based standardization during this time from
case 350 to 400 contributed to a marked decrease in thoracoscopic operative time (by almost 30 min),
even though the number of surgeries performed by less experienced operators increased. We believe that
accurate understanding of the microanatomy involved contributed towards defining the surgical planes
more easily for quick dissection of tissues including the lymph nodes with without extra bleeding. On
the other hand, young surgeons could also learn the microanatomy from experienced surgeons through