Page 15 - Read Online
P. 15
M’Harzi et al. Mini-invasive Surg 2019;3:27 I http://dx.doi.org/10.20517/2574-1225.2019.22 Page 5 of 7
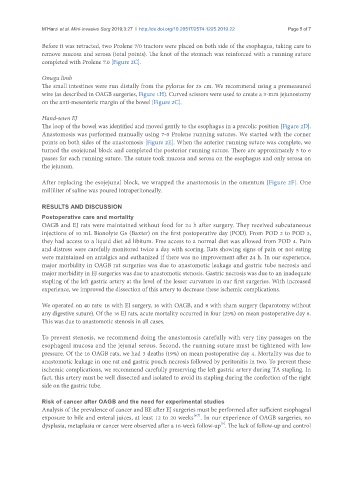
Before it was retracted, two Prolene 7/0 tractors were placed on both side of the esophagus, taking care to
remove mucosa and serosa (total points). The knot of the stomach was reinforced with a running suture
completed with Prolene 7.0 [Figure 2C].
Omega limb
The small intestines were run distally from the pylorus for 25 cm. We recommend using a premeasured
wire (as described in OAGB surgeries, Figure 1H). Curved scissors were used to create a 3-mm jejunostomy
on the anti-mesenteric margin of the bowel [Figure 2C].
Hand-sewn EJ
The loop of the bowel was identified and moved gently to the esophagus in a precolic position [Figure 2D].
Anastomosis was performed manually using 7-0 Prolene running sutures. We started with the corner
points on both sides of the anastomosis [Figure 2E]. When the anterior running suture was complete, we
turned the esojejunal block and completed the posterior running suture. There are approximately 5 to 6
passes for each running suture. The suture took mucosa and serosa on the esophagus and only serosa on
the jejunum.
After replacing the esojejunal block, we wrapped the anastomosis in the omentum [Figure 2F]. One
milliliter of saline was poured intraperitoneally.
RESULTS AND DISCUSSION
Postoperative care and mortality
OAGB and EJ rats were maintained without food for 24 h after surgery. They received subcutaneous
injections of 10 mL Bionolyte G5 (Baxter) on the first postoperative day (POD). From POD 2 to POD 3,
they had access to a liquid diet ad libitum. Free access to a normal diet was allowed from POD 4. Pain
and distress were carefully monitored twice a day with scoring. Rats showing signs of pain or not eating
were maintained on antalgics and euthanized if there was no improvement after 24 h. In our experience,
major morbidity in OAGB rat surgeries was due to anastomotic leakage and gastric tube necrosis and
major morbidity in EJ surgeries was due to anastomotic stenosis. Gastric necrosis was due to an inadequate
stapling of the left gastric artery at the level of the lesser curvature in our first surgeries. With increased
experience, we improved the dissection of this artery to decrease these ischemic complications.
We operated on 40 rats: 16 with EJ surgery, 16 with OAGB, and 8 with sham surgery (laparotomy without
any digestive suture). Of the 16 EJ rats, acute mortality occurred in four (25%) on mean postoperative day 6.
This was due to anastomotic stenosis in all cases.
To prevent stenosis, we recommend doing the anastomosis carefully with very tiny passages on the
esophageal mucosa and the jejunal serous. Second, the running suture must be tightened with low
pressure. Of the 16 OAGB rats, we had 3 deaths (19%) on mean postoperative day 4. Mortality was due to
anastomotic leakage in one rat and gastric pouch necrosis followed by peritonitis in two. To prevent these
ischemic complications, we recommend carefully preserving the left gastric artery during TA stapling. In
fact, this artery must be well dissected and isolated to avoid its stapling during the confection of the right
side on the gastric tube.
Risk of cancer after OAGB and the need for experimental studies
Analysis of the prevalence of cancer and BE after EJ surgeries must be performed after sufficient esophageal
[6,7]
exposure to bile and enteral juices, at least 12 to 20 weeks . In our experience of OAGB surgeries, no
[5]
dysplasia, metaplasia or cancer were observed after a 16-week follow-up . The lack of follow-up and control