Page 231 - Read Online
P. 231
to periodontal/dental infection and disease, will lead to
exposure of the alveolar bone, which may already be necrotic
and will not heal. Infection, within a unifying concept
[17]
of medication-related impaired immune response was
proposed to play an important role in the pathophysiology
of ONJ. [18]
In this paper we report what we believe is the first case of
ONJ in a patient with acute myeloid leukemia (AML), who
was treated with azacitidine. The presence of alveolar bone
disease leads to the dental extraction and the subsequent
diagnosis of ONJ.
CASE REPORT
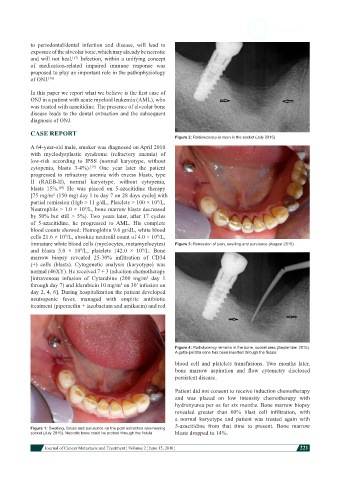
Figure 2: Radiolucency is seen in the socket (July 2015)
A 64-year-old male, smoker was diagnosed on April 2010
with myelodysplastic syndrome (refractory anemia) of
low-risk according to IPSS (normal karyotype, without
cytopenia, blasts 3-4%). One year later the patient
[19]
progressed to refractory anemia with excess blasts, type
II (RAEB-II), normal karyotype, without cytopenia,
blasts 15%. He was placed on 5-azacitidine therapy
[20]
[75 mg/m (150 mg) day 1 to day 7 on 28 days cycle] with
2
partial remission (Hgb > 11 g/dL, Platelets > 100 × 10 /L,
9
Neutrophils > 1.0 × 10 /L, bone marrow blasts decreased
9
by 50% but still > 5%). Two years later, after 17 cycles
of 5-azacitidine, he progressed to AML. His complete
blood counts showed: Hemoglobin 9.6 gr/dL, white blood
cells 21.6 × 10 /L, absolute neutrofil count of 4.0 × 10 /L,
9
9
immature white blood cells (myelocytes, metamyelocytes) Figure 3: Remission of pain, swelling and purulence (August 2015)
and blasts 5.0 × 10 /L, platelets 142.0 × 10 /L. Bone
9
9
marrow biopsy revealed 25-30% infiltration of CD34
(+) cells (blasts). Cytogenetic analysis (karyotype) was
normal (46XY). He received 7 + 3 induction chemotherapy
[intravenous infusion of Cytarabine (200 mg/m day 1
2
through day 7) and Idarubicin 10 mg/m on 30’ infusion on
2
day 2, 4, 6]. During hospitalization the patient developed
neutropenic fever, managed with empiric antibiotic
treatment (piperacilin + tazobactam and amikacin) and red
Figure 4: Radiolucency remains in the bone, socket area (September 2015).
A gutta-percha cone has been inserted through the fistula
blood cell and platelets transfusions. Two months later,
bone marrow aspiration and flow cytometry disclosed
persistent disease.
Patient did not consent to receive induction chemotherapy
and was placed on low intensity chemotherapy with
hydroxyurea per os for six months. Bone marrow biopsy
revealed greater than 60% blast cell infiltration, with
a normal karyotype and patient was treated again with
5-azacitidine from that time to present. Bone marrow
Figure 1: Swelling, fistula and purulunce on the post extraction non-healing
socket (July 2015). Necrotic bone could be probed through the fistula blasts dropped to 14%.
Journal of Cancer Metastasis and Treatment ¦ Volume 2 ¦ June 15, 2016 ¦ 221