Page 105 - Read Online
P. 105
Page 8 of 19 Davidson et al. J Cancer Metastasis Treat 2021;7:45 https://dx.doi.org/10.20517/2394-4722.2021.77
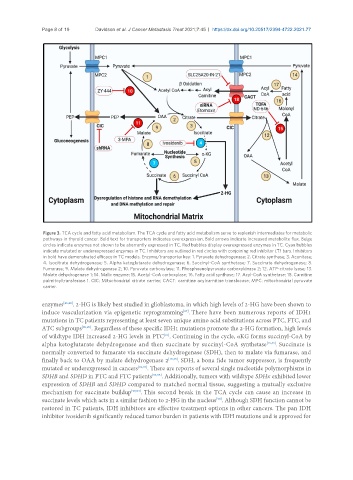
Figure 3. TCA cycle and fatty acid metabolism. The TCA cycle and fatty acid metabolism serve to replenish intermediates for metabolic
pathways in thyroid cancer. Bold text for transporters indicates overexpression. Bold arrows indicate increased metabolite flux. Beige
circles indicate enzymes not shown to be aberrantly expressed in TC. Red bubbles display overexpressed enzymes in TC. Cyan bubbles
indicate mutated or underexpressed enzymes in TC. Inhibitors are outlined in red circles with conjoining red inhibitor (T) bars. Inhibitors
in bold have demonstrated efficacy in TC models. Enzyme/transporter key: 1. Pyruvate dehydrogenase; 2. Citrate synthase; 3. Aconitase;
4. Isocitrate dehydrogenase; 5. Alpha ketoglutarate dehydrogenase; 6. Succinyl-CoA synthetase; 7. Succinate dehydrogenase; 8.
Fumarase; 9. Malate dehydrogenase 2; 10. Pyruvate carboxylase; 11. Phosphoenolpyruvate carboxykinase 2; 12. ATP-citrate lyase; 13.
Malate dehydrogenase 1; 14. Malic enzyme; 15. Acetyl-CoA carboxylase; 16. Fatty acid synthase; 17. Acyl-CoA synthetase; 18. Carnitine
palmitoyltransferase 1. CIC: Mitochondrial citrate carrier; CACT: carnitine acylcarnitine translocase; MPC: mitochondrial pyruvate
carrier.
enzymes [86,88] . 2-HG is likely best studied in glioblastoma, in which high levels of 2-HG have been shown to
induce vascularization via epigenetic reprogramming . There have been numerous reports of IDH1
[87]
mutations in TC patients representing at least seven unique amino acid substitutions across PTC, FTC, and
ATC subgroups [89,90] . Regardless of these specific IDH1 mutations promote the 2-HG formation, high levels
of wildtype IDH increased 2-HG levels in PTC . Continuing in the cycle, αKG forms succinyl-CoA by
[91]
alpha ketoglutarate dehydrogenase and then succinate by succinyl-CoA synthetase [15,35] . Succinate is
normally converted to fumarate via succinate dehydrogenase (SDH), then to malate via fumarase, and
finally back to OAA by malate dehydrogenase 2 [15,35] . SDH, a bona fide tumor suppressor, is frequently
mutated or underexpressed in cancers [92,93] . There are reports of several single nucleotide polymorphisms in
SDHB and SDHD in PTC and FTC patients [94,95] . Additionally, tumors with wildtype SDHx exhibited lower
expression of SDHB and SDHD compared to matched normal tissue, suggesting a mutually exclusive
mechanism for succinate buildup [93,94] . This second break in the TCA cycle can cause an increase in
succinate levels which acts in a similar fashion to 2-HG in the nucleus . Although SDH function cannot be
[93]
restored in TC patients, IDH inhibitors are effective treatment options in other cancers. The pan IDH
inhibitor ivosidenib significantly reduced tumor burden in patients with IDH mutations and is approved for