Page 47 - Read Online
P. 47
Table 1: Pre-operative imaging studies
Diagnostic study Number of studies Median days pre-LT Sensitivity (%) NPV (%) Specificity (%) PPV (%)
US (no flow = PVT) 149 26 4.8 13.8 97.7 25.0
US (no, diminished, or 149 26 31.6 10.5 85.4 24.0
reversal of flow = PVT)
CT 158 56.5 19.0 11.2 98.5 66.7
MRI 51 66 12.5 14.3 97.7 50.0
RPV 11 45 50.0 22.2 100.0 100.0
The efficacy of pre-operative diagnostic studies has long been questioned. Our data support this as well. Even when we set criteria for ultrasound diagnosis
liberally (2nd US row), the sensitivity and NPV were wholly inadequate. Though the number is small, in our series even RPV, a direct and invasive technique
only detected PVT pre-LT in half the cases. LT: liver transplant; PVT: portal vein thrombosis; NPV: negative predictive value; PPV: positive predictive value;
RPV: retrograde portal venography; US: ultrasound
Table 2: Variables related to PVT
Perioperative variables PVT No PVT P
Pre-operative variables
Age 57.8 53.8 0.041
Gender: female 23.3% 33.3% NS
Non-Caucasian race 30.0% 29.0% NS
Medicare or medicaid 20.0% 43.0% NS
Hepatocellular carcinoma 2.8% 13.6% NS
diagnosis
Hepatitis C virus diagnosis 50.0% 52.7% NS
MELD 25.0 21.4 0.049
Cr 1.6 1.8 NS
Total bilirubin 7.2 5.0 NS
INR 2.0 1.8 NS
Pre-LT ICU status 30.0% 15.6% 0.07
Pre-LT hemodialysis 26.7% 15.6% NS
Previous upper abdominal surgery 30.0% 25.8% NS
Intra- and post-operative variables
Cold ischemic time 367.7 350.2 NS
Warm ischemic time 35.9 34.4 NS
PRBC 28.9 17.5 0.001
Reentry 40.0% 36.0% NS
Morbidity (≥ Clavien II) 43.3% 37.6% NS
LOS, total (days) 19.8 16.6 NS
Age, MELD score, and the amount of blood loss were greater in patients
who had PVT (bold print signifies significant values). The proportion of
patients in the ICU with PVT was greater but only approached statistical
significance. With logistic regression, the only pre-operative factor
independently associated with PVT was age (P = 0.037/HR = 0.95). Pre-LT:
pre-liver transplant; LOS: length of stay; PVT: portal vein thrombosis; ICU:
intensive care unit; MELD: model for end-stage liver disease; PRBC: packed
red blood cell; HR: hazard ratio; NS: not significant
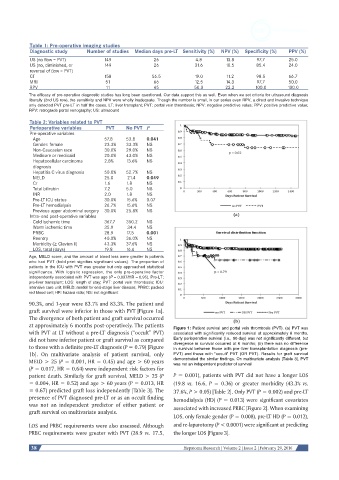
90.3%, and 1-year were 83.7% and 83.3%. The patient and
graft survival were inferior in those with PVT [Figure 1a].
The divergence of both patient and graft survival occurred
at approximately 6 months post-operatively. The patients Figure 1: Patient survival and portal vein thrombosis (PVT). (a) PVT was
with PVT at LT without a pre-LT diagnosis (“occult” PVT) associated with significantly reduced survival at approximately 6 months.
did not have inferior patient or graft survival as compared Early perioperative survival (i.e., 90-day) was not significantly different, but
to those with a definite pre-LT diagnosis (P = 0.79) [Figure divergence in survival occurred at 6 months; (b) there was no difference
in survival between those with pre-liver transplantation diagnosis (pre-
1b]. On multivariate analysis of patient survival, only PVT) and those with “occult” PVT (OR PVT). Results for graft survival
MELD > 25 (P = 0.001, HR = 0.45) and age > 60 years demonstrated the similar findings. On multivariate analysis [Table 3], PVT
was not an independent predictor of survival
(P = 0.017, HR = 0.64) were independent risk factors for
patient death. Similarly for graft survival, MELD > 25 (P P = 0.001), patients with PVT did not have a longer LOS
= 0.004, HR = 0.52) and age > 60 years (P = 0.013, HR (19.8 vs. 16.6, P = 0.36) or greater morbidity (43.3% vs.
= 0.67) predicted graft loss independently [Table 3]. The 37.6%, P > 0.05) [Table 2]. Only PVT (P = 0.002) and pre-LT
presence of PVT diagnosed pre-LT or as an occult finding hemodialysis (HD) (P = 0.013) were significant covariates
was not an independent predictor of either patient or associated with increased PRBC [Figure 2]. When examining
graft survival on multivariate analysis.
LOS, only female gender (P = 0.008), pre-LT HD (P = 0.012),
LOS and PRBC requirements were also assessed. Although and re-laparotomy (P < 0.0001) were significant at predicting
PRBC requirements were greater with PVT (28.9 vs. 17.5, the longer LOS [Figure 3].
38 Hepatoma Research | Volume 2 | Issue 2 | February 29, 2016