Page 96 - Read Online
P. 96
Xu et al. Art Int Surg 2023;3:48-63 https://dx.doi.org/10.20517/ais.2022.33 Page 54
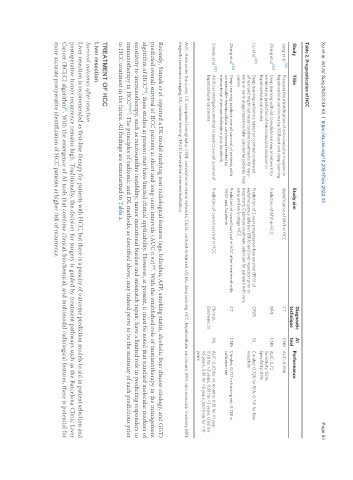
Table 2. Prognostication of HCC
Diagnostic AI
Study Title Study aim Performance
technique tool
[55]
Jiang et al. Preoperative identification of microvascular invasion in Identification of MVI in HCC CT CNN AUC: 0.906
hepatocellular carcinoma by XGBoost and deep learning
[56]
Zhang et al. Deep learning with 3d convolutional neural network for Prediction of MVI in HCC MRI CNN AUC: 0.72
noninvasive prediction of microvascular invasion in Sensitivity: 55%
hepatocellular carcinoma Specificity: 81%
[57]
Liu et al. Deep learning radiomics based on contrast-enhanced Prediction of 2-year progression-free survival (PFS) of CEUS DL C-index: 0.726 for RFA, 0.741 for liver
ultrasound might optimize curative treatments for very- radiofrequency ablation (RFA) and liver resection prior to resection
early or early-stage hepatocellular carcinoma patients. liver treatment; Optimize treatment selection for patients with very
cancer early and early-stage HCC
[58]
Zhang et al. Deep Learning predicts overall survival of patients with Prediction of overall survival in HCC after treatment with CT CNN C-index: 0.717 in training set, 0.714 in
unresectable hepatocellular carcinoma treated by TACE and Sorafenib validation set
transarterial chemoembolization plus Sorafenib
Simsek et al. [23] Artificial intelligence method to predict overall survival of Prediction of overall survival in HCC Clinical, ML AUC: 0.92 for >6 months, 0.81 for >1 year,
hepatocellular carcinoma Biochemical 0.78 for >2 years, 0.81 for >3 years, 0.82 for
>5 years, 0.81 for >8 years, and 0.66 for >10
years
AUC: Area under the curve; CT: computed tomography; CNN: convolutional neural networks; CEUS: contrast-enhanced US; DL: deep learning HCC: hepatocellular carcinoma; MVI: microvascular invasion; MRI:
magnetic resonance imaging; ML: machine learning; TACE: transarterial chemoembolization.
Recently, Simsek et al. reported a DL model studying non-radiological features (age, bilirubin, AFP, smoking status, alcoholic liver disease etiology, and GGT)
predicted overall survival of HCC patients at short and long-term intervals (AUC 0.92) . With the established role of immunotherapy in the management
[23]
algorithm of HCC , these studies at present may have limited clinical applicability. However, at present, it must be noted that standard molecular markers of
[63]
sensitivity to immunotherapy, such as microsatellite instability, tumor mutational burden and mismatch repair, have a limited role in predicting responders to
immunotherapy in HCC [64,65] . The principles of radiomic and DL methods, as described above, may indeed prove to be the mainstay of such predictions prior
to HCC treatment in the future. All findings are summarized in Table 2.
TREATMENT OF HCC
Liver resection
Survival outcomes after resection
Liver resection is recommended as first-line therapy for patients with HCC, but there is a paucity of outcome prediction models to aid in patient selection and
postoperative tumor recurrence remains high. Traditionally, the decision for surgery is guided by treatment pathways such as the Barcelona Clinic Liver
Cancer (BCLC) algorithm . With the emergence of AI tools that combine clinical, biochemical, and multimodal radiological features, there is potential for
[2]
more accurate preoperative identification of HCC patients at higher risk of recurrence.