Page 392 - Read Online
P. 392
Page 10 of 13 Pisano et al. Vessel Plus 2020;4:33 I http://dx.doi.org/10.20517/2574-1209.2020.21
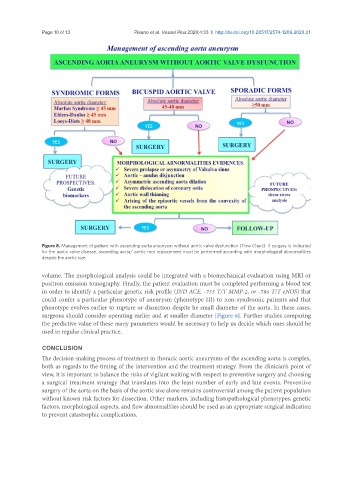
Figure 8. Management of patient with ascending aorta aneurysm without aortic valve dysfunction (Flow Chart). If surgery is indicated
for the aortic valve disease, ascending aorta/ aortic root replacement must be performed according with morphological abnormalities
despite the aortic size
volume. The morphological analysis could be integrated with a biomechanical evaluation using MRI or
positron emission tomography. Finally, the patient evaluation must be completed performing a blood test
in order to identify a particular genetic risk profile (D/D ACE, -735 T/T MMP-2, or -786 T/T eNOS) that
could confer a particular phenotype of aneurysm (phenotype III) to non-syndromic patients and that
phenotype evolves earlier to rupture or dissection despite he small diameter of the aorta. In these cases,
surgeons should consider operating earlier and at smaller diameter [Figure 8]. Further studies comparing
the predictive value of these many parameters would be necessary to help us decide which ones should be
used in regular clinical practice.
CONCLUSION
The decision-making process of treatment in thoracic aortic aneurysms of the ascending aorta is complex,
both as regards to the timing of the intervention and the treatment strategy. From the clinician’s point of
view, it is important to balance the risks of vigilant waiting with respect to preventive surgery and choosing
a surgical treatment strategy that translates into the least number of early and late events. Preventive
surgery of the aorta on the basis of the aortic size alone remains controversial among the patient population
without known risk factors for dissection. Other markers, including histopathological phenotypes, genetic
factors, morphological aspects, and flow abnormalities should be used as an appropriate surgical indication
to prevent catastrophic complications.