Page 126 - Read Online
P. 126
Carr et al. Vessel Plus 2020;4:12 I http://dx.doi.org/10.20517/2574-1209.2020.01 Page 7 of 21
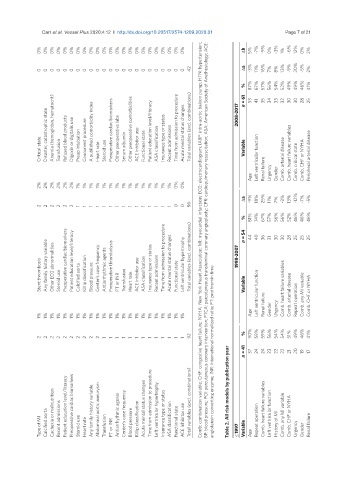
BP: blood pressure; PCI: percutaneous coronary intervention; PTCA: percutaneous transluminal coronary angioplasty; CPR: cardiopulmonary resuscitation; ASA: American Society of Anethesiology; ACE:
Comb: combination variable; CHF: congestive heart failure; NYHA: New York Heart Association; MI: myocardial infarction; ECG: electrocardiogram; IABP: intra-aortic baloon pump; HTN: hypertension;
0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% Δb 5% -7% -9% 0% -3% 1% -6% 12% 0% 2%
42 Δa -3% 11% 16% 8% 13% -9% 20% -5%
0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 7% 2%
87% 67% 56% 54% 52% 49% 49% 46%
% n = 61 53 41 57% 35 34 33 32 30 30 28 41% 25
Disaster, catastrophic state Anemia (hemoglobin, hematocrit) Refused blood products Digoxin or digitalis use Concurrent procedure A published comorbidity index Preoperative cardiac biomarkers Other preoperative labs Other preoperative comorbidities Patient education level/literacy Insurance type or status Time from admission to procedure Acute mental status changes Total variables (excl. combinations) 2008-2017
Critical state Transfusion Preop intubation Heart rate Steroid use Serum albumin ACE inhibitor use Functional state ASA classification Recent admissions Variable Left ventricular function Comb. arterial disease Comb. heart failure variables Comb. critical state Comb. CHF or NYHA Peripheral arterial disease
Age Renal failure Urgency Gender
2% 2% 2% 2% 2% 2% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 0% 0%
Δa -9% 18% 25% 11% 7% -3% 13% -12% -7% -5%
2 2 2 2 2 2 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 0 0 90
% n = 54 81% 44 74% 40 67% 36 57% 31 56% 30 56% 30 52% 28 46% 25 46% 25 46% 25
Stent thrombosis Any family history variable Other ECG abnormalities Steroid use Preoperative cardiac biomarkers Patient education level/literacy Calcified aorta Killip classification Blood pressure Center’s case frequency Antiarrhythmic agents Preoperative thrombolysis PT or INR Transfusion Heart rate ACE inhibitor use ASA classification Insurance type or status Recent admissions Time from admission to procedure Acute mental status changes
Age Renal failure Gender Urgency Comb. arterial disease Repeat operation Comb. any MI variable Comb. CHF or NYHA
1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1% 1%
2 2 2 2 2 2 2 2 2 2 1 1 1 1 1 1 1 1 1 1 1 1 1 92 angiotensin converting enzyme; INR: international normalized ratio; PT: prothromin time % n = 41 90% 37 59% 24 59% 24 56% 23 54% 22 54% 22 51% 21 49% 20 46% 19 41% 17
Type of MI Calcified aorta Cachexia or malnutrition Recent admissions Patient education level/literacy Preoperative cardiac biomarkers Steroid use Heart rate Any family history variable Abdominal aortic aneurysm Transfusion PT or INR Antiarrhythmic agents Center’s case frequency Blood pressure Killip classification Acute mental status changes Time from admission to procedure Left ventricular hypertrophy Insurance type or status ASA classificat