Page 80 - Read Online
P. 80
Rademacher et al. Vessel Plus 2022;6:39 https://dx.doi.org/10.20517/2574-1209.2021.138 Page 5 of 9
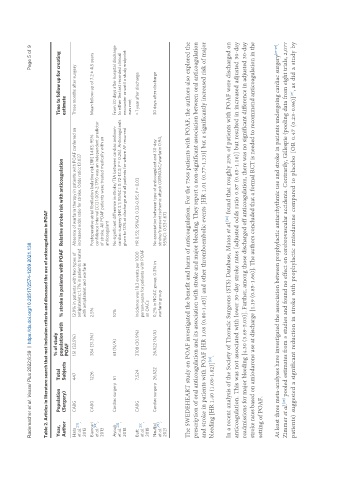
Table 2. Articles in literature search that met inclusion criteria and discussed the use of anticoagulation in POAF
% of study
Year, Population Total Time to follow up for creating
Author (Surgery) Subjects population with % stroke in patients with POAF Relative stroke risk with anticoagulation estimate
POAF
Hata CABG 447 151 (33.5%) 12.9% in patients with two types of Absence of warfarin therapy in patients with POAF conferred an Three months after surgery
[21]
et al. , antiplatelets; 1.7% in patients treated increased odds ratio for stroke. Odds ratio: 13.037
2013 with antiplatelet and warfarin
Biancari CABG 1226 384 (31.3%) 2.5% Postoperative atrial fibrillation (relative risk [RR] 1.483; 95% Mean follow-up of 7.2 ± 4.5 years
et al. [24] , confidence interval [CI] 1.009-2.179) was an independent predictor
2013 of stroke. All POAF patients were treated medically with an
anticoagulant
Ayoub Cardiac surgery 61 61 (N/A) 10% No significant difference in stroke/TIA between cardiac and non- From 30 days after hospital discharge
[23]
et al. , cardiac surgery (HR 3.1; 95%CI: 0.72-13.3; P = 0.26). Anticoagulants to either the last recorded clinical
2018 given to 13% at discharge and all patients for whom AF recurred encounter or until a study endpoint
was met
Butt CABG 7,524 2108 (30.9%) Incidence was 18.3 events per 1000 HR 0.55; 95%CI: 0.32-0.95; P = 0.03 > 1 year after discharge
[33]
et al. , person-years for patients with POAF
2018 on OACs
Nauffal Cardiac surgery 26,522 26,522 (N/A) 0.2% in NOAC group, 0.3% in No association between type of anticoagulant and 30-day 30 days after discharge
et al. [20] , warfarin group stroke/transient ischemic attack (ORNOAC/warfarin 0.94,
2021 95%CI: 0.53-1.67)
The SWEDEHEART study on POAF investigated the benefit and harm of anticoagulation. For the 7368 patients with POAF, the authors also explored the
prescription of oral anticoagulation and its association with stroke and major bleeding. They report a non-significant association between oral anticoagulation
and stroke in patients with POAF [HR 1.08 (0.80-1.45)] and other thromboembolic events [HR 1.01 (0.77-1.33)] but a significantly increased risk of major
[19]
bleeding [HR 1.40 (1.08-1.82)] .
In a recent analysis of the Society of Thoracic Surgeons (STS) Database, Matos et al. found that roughly 25% of patients with POAF were discharged on
[26]
anticoagulation. This was not associated with lower 30-day stroke rates [adjusted odds ratio 0.87 (0.65-1.16)] but resulted in increased adjusted 30-day
readmissions for major bleeding [4.30 (3.69-5.03)]. Further, among those discharged off anticoagulation, there was no significant difference in adjusted 30-day
stroke rates based on amiodarone use at discharge [1.19 (0.85-1.66)]. The authors concluded that a formal RCT is needed to recommend anticoagulation in the
setting of POAF.
At least three meta-analyses have investigated the association between prophylactic antiarrhythmic use and stroke in patients undergoing cardiac surgery [27-29] .
Zimmer et al. pooled estimates from 5 studies and found no effect on cerebrovascular accidents. Contrarily, Gillespie (pooling data from eight trials, 2,077
[28]
[29]
patients) suggested a significant reduction in stroke with prophylactic amiodarone compared to placebo [OR 0.47 (0.23-0.96)] , as did a study by