Page 67 - Read Online
P. 67
Dokko et al. Vessel Plus 2022;6:37 https://dx.doi.org/10.20517/2574-1209.2021.121 Page 13 of 21
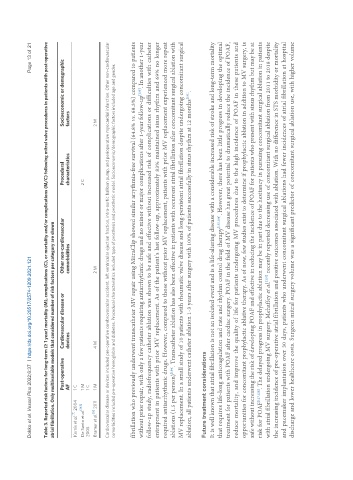
Table 3. Reported risk factors for long-term (≥ 1 year) mortality (M), complications (C), or mortality and/or complications (M/C) following mitral valve procedures in patients with post-operative
atrial fibrillation. Only multivariable models that considered number of risk factors per category are shown
Post-operative Cardiovascular disease or Other non-cardiovascular Procedural Socioeconomic or demographic
AF devices comorbidities characteristics factors
[7]
Kernis et al. 2004 1 C
De Santo et al. [163] 1 M 2 C
2005 1 C
[6]
Bramer et al. 2011 1 M 4 M 2 M 2 M
Cardiovascular disease or devices included pre-operative cerebrovascular accident, left ventricular ejection fraction, intra-aortic balloon pump, and perioperative myocardial infarction. Other non-cardiovascular
comorbidities included pre-operative hemoglobin and diabetes. Procedural characteristics included type of prosthesis and prosthetic model. Socioeconomic/demographic factors included age and gender.
fibrillation who previously underwent transcatheter MV repair using MitraClip showed similar arrythmia-free survival (64.8% vs. 68.3%) compared to patients
without prior repair, with only a few patients requiring antiarrhythmic drugs and no minor or major complications after 1-year follow-up . In another 1-year
[133]
follow-up study, radiofrequency catheter ablation was shown to be safe and effective without increased risk of complications or difficulties with catheter
entrapment in patients with prior MV replacement. As of the patient’s last follow-up, approximately 83% maintained sinus rhythm and 69% no longer
required antiarrhythmic drugs. However, compared to those without prior MV replacement, patients with prior MV replacement experienced more repeat
[134]
ablations (1.5 per person) . Transcatheter ablation has also been effective in patients with recurrent atrial fibrillation after concomitant surgical ablation with
MV replacement. In a small study of 10 patients with rheumatic valve disease and long-persistent atrial fibrillation despite undergoing concomitant surgical
ablation, all patients underwent catheter ablation 1-3 years after surgery with 100% of patients successfully in sinus rhythm at 12 months .
[131]
Future treatment considerations
It is well known that atrial fibrillation is not an isolated event and is a life-altering disease with a considerable increased risk of stroke and long-term mortality
that requires life-long anticoagulation and rate and rhythm control drug therapy [135,136] . However, there has been little progress in developing the optimal
treatment for patients with POAF after cardiac surgery. POAF in the field of MV disease has great potential to dramatically reduce the incidence of POAF,
reduce mortality, and improve the quality of life for patients undergoing MV procedures due to the high incidence of POAF in these patients and
opportunities for concomitant prophylactic ablative therapy. As of now, few studies exist to determine if prophylactic ablation in addition to MV surgery, is
safe without increasing the risk of developing POAF and effective in reducing the incidence of POAF for patients who present with sinus rhythm but may be at
risk for POAF [127,128] . The delayed progress in prophylactic ablation may be in part due to the hesitancy in pursuing concomitant surgical ablation in patients
[137]
with atrial fibrillation undergoing MV surgery. Mehaffey et al. recently reported decreasing use of concomitant surgical ablation from 2011 to 2018 despite
the increasing incidence of pre-operative atrial fibrillation and positive outcomes associated with ablation. With no difference in STS morbidity or mortality
and pacemaker implantation over 30 days, patients who underwent concomitant surgical ablations had fewer incidences of atrial fibrillation at hospital
discharge and lower healthcare costs. Surgeon mitral surgery volume was a significant predictor of concomitant surgical ablation use, with higher volume