Page 21 - Read Online
P. 21
Padoan et al. Vessel Plus 2021;5:41 https://dx.doi.org/10.20517/2574-1209.2021.41 Page 3 of 18
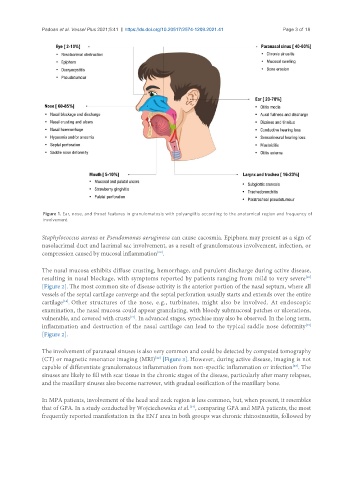
Figure 1. Ear, nose, and throat features in granulomatosis with polyangiitis according to the anatomical region and frequency of
involvement.
Staphylococcus aureus or Pseudomonas aeruginosa can cause cacosmia. Epiphora may present as a sign of
nasolacrimal duct and lacrimal sac involvement, as a result of granulomatous involvement, infection, or
compression caused by mucosal inflammation .
[20]
The nasal mucosa exhibits diffuse crusting, hemorrhage, and purulent discharge during active disease,
[19]
resulting in nasal blockage, with symptoms reported by patients ranging from mild to very severe
[Figure 2]. The most common site of disease activity is the anterior portion of the nasal septum, where all
vessels of the septal cartilage converge and the septal perforation usually starts and extends over the entire
cartilage . Other structures of the nose, e.g., turbinates, might also be involved. At endoscopic
[14]
examination, the nasal mucosa could appear granulating, with bloody submucosal patches or ulcerations,
vulnerable, and covered with crusts . In advanced stages, synechiae may also be observed. In the long term,
[21]
inflammation and destruction of the nasal cartilage can lead to the typical saddle nose deformity
[19]
[Figure 2].
The involvement of paranasal sinuses is also very common and could be detected by computed tomography
[22]
(CT) or magnetic resonance imaging (MRI) [Figure 3]. However, during active disease, imaging is not
capable of differentiate granulomatous inflammation from non-specific inflammation or infection . The
[23]
sinuses are likely to fill with scar tissue in the chronic stages of the disease, particularly after many relapses,
and the maxillary sinuses also become narrower, with gradual ossification of the maxillary bone.
In MPA patients, involvement of the head and neck region is less common, but, when present, it resembles
that of GPA. In a study conducted by Wojciechowska et al. , comparing GPA and MPA patients, the most
[24]
frequently reported manifestation in the ENT area in both groups was chronic rhinosinusitis, followed by