Page 101 - Read Online
P. 101
West et al. Rare Dis Orphan Drugs J 2024;3:22 https://dx.doi.org/10.20517/rdodj.2023.61 Page 13 of 34
Table 3. Kidney diseases with lamellar bodies
Condition Reference
Fabry disease Gubler et al., 1978 [80]
[84]
Drug-induced renal phospholipidosis Reasor et al., 2006
[85]
Neimann-Pick disease Grafft et al., 2009
[86]
Silicosis Banks et al., 1983
[87]
LMX1B-associated nephropathy (nail patella syndrome) Lei et al., 2020
LCAT deficiency Hirashio et al., 2014 [88]
[89]
CoQ2 nephropathy Ni et al., 2021
Radiocontrast Su et al., 2018 [90]
[91]
Renal cell carcinoma Hull et al., 1988
Idiopathic Kadosawa et al., 2020 [92]
LCAT: Lecithin cholesterol acyltransferase; CoQ2: co-enzyme Q2.
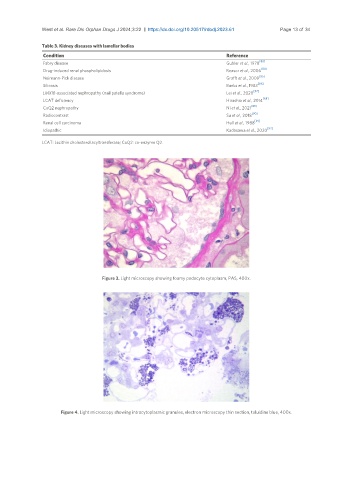
Figure 3. Light microscopy showing foamy podocyte cytoplasm, PAS, 400x.
Figure 4. Light microscopy showing intracytoplasmic granules, electron microscopy thin section, toluidine blue, 400x.