Page 70 - Read Online
P. 70
Sears et al. Plast Aesthet Res 2024;11:31 https://dx.doi.org/10.20517/2347-9264.2024.04 Page 3 of 5
Table 1. Summary of neural interfaces for prosthetic control that rely on nerve regeneration for prosthetic actuation
Versatility for
Interfacing
Method Functionality neural Summary
tissue interfacing
TMR Skin Motor Upper Limb The terminal end of a transected nerve reinnervates the intact proximal muscles.
High-density surface EMG electrode grids enable the recording of motor unit
activity across 64 channels
RPNI Skin Or Motor and Upper and The transected nerve is divided into several subunits, each reinnervating a muscle
Muscle Sensation Lower Limb graft harvested from a proximal donor site. This biological PNI can be recorded or
stimulated using transcutaneous or percutaneous electrodes. The number of
available recording and stimulating channels is defined by the number of nerve
subunits and the interface method
Sieve Fascicles Motor and Upper and The flat, porous structure of sieve electrodes presents discrete microchannels to
electrode Sensation Lower Limb isolate regenerating axons of the transected nerve. Double-layering allows for 64
channels capable of recording and stimulating specific fascicles
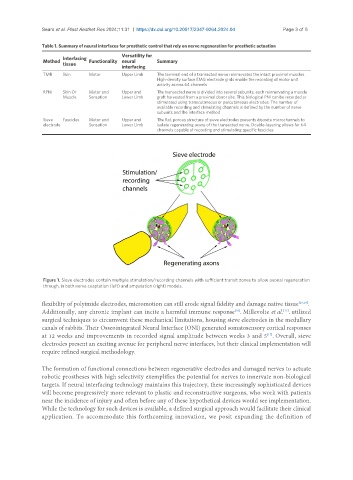
Figure 1. Sieve electrodes contain multiple stimulation/recording channels with sufficient transit zones to allow axonal regeneration
through, in both nerve coaptation (left) and amputation (right) models.
flexibility of polyimide electrodes, micromotion can still erode signal fidelity and damage native tissue [15,16] .
Additionally, any chronic implant can incite a harmful immune response . Millevolte et al. . utilized
[16]
[17]
surgical techniques to circumvent these mechanical limitations, housing sieve electrodes in the medullary
canals of rabbits. Their Osseointegrated Neural Interface (ONI) generated somatosensory cortical responses
at 12 weeks and improvements in recorded signal amplitude between weeks 3 and 5 . Overall, sieve
[17]
electrodes present an exciting avenue for peripheral nerve interfaces, but their clinical implementation will
require refined surgical methodology.
The formation of functional connections between regenerative electrodes and damaged nerves to actuate
robotic prostheses with high selectivity exemplifies the potential for nerves to innervate non-biological
targets. If neural interfacing technology maintains this trajectory, these increasingly sophisticated devices
will become progressively more relevant to plastic and reconstructive surgeons, who work with patients
near the incidence of injury and often before any of these hypothetical devices would see implementation.
While the technology for such devices is available, a defined surgical approach would facilitate their clinical
application. To accommodate this forthcoming innovation, we posit expanding the definition of